In a comparison with screening mammography, molecular breast imaging (MBI) showed high sensitivity and specificity in women with a high risk of cancer and could provide a less expensive imaging option to MRI.
Researchers at the Mayo Clinic in Rochester, MN, undertook the study to evaluate MBI as a screening technique in women at increased risk of developing breast cancer. "Screening is all about early breast cancer detection," said study co-author Michael O'Connor, Ph.D., from the department of nuclear medicine at the Mayo Clinic. "You are not going to be in the game unless you can reliably detect lesions in the range of 5 to 15 mm in size."
The study, funded by the Susan G. Komen Foundation, reviewed 800 women at increased risk of breast cancer between September 2005 and December 2007 who underwent MBI and screening mammography. Of the initial 800 women in the study, 762 were included in the final analysis.
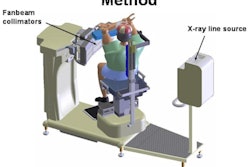
Patients were injected with 740 MBq technetium-99m sestamibi. Craniocaudal and mediolateral oblique images of each breast were obtained, with the scan beginning 15 minutes after injection. For the imaging procedures, researchers used what O'Connor described as "light, pain-free" compression at about one-third the compression force of mammography (15 lb of force versus 45 lb of force).
Modified camera
To perform molecular breast imaging, researchers used a dual-head semiconductor-based gamma camera technology under development at Mayo for the past five years. The two detectors are mounted on the modified gamma camera to optimize the breast image to the very edge of the breast.
O'Connor, who presented study results at the annual SNM meeting, said the new system has image resolution of approximately 1.625 mm; can perform quantification of tumor depth, size, and uptake; and "is two to three times better than a conventional gamma camera."
"Our goal was to replicate some of the other studies that looked at patients with increased risk of breast cancer," he added. "Basically, we wanted to image patients who were asymptomatic, had increased risk of breast cancer for a variety of reasons, and they had to have a greater than 50% dense pattern on their mammogram. Increased breast density confers the increased risk of breast cancer."
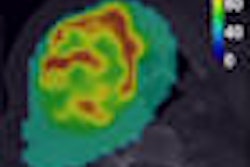
Cancer detection
To date, a total of 10 cancers in nine patients were diagnosed. Molecular breast imaging detected cancer in eight of 10 patients, while mammography found cancer in three of 10 patients. The majority of discovered tumors were 10 mm or smaller in size, which, O'Connor said, is very important "given the fact that conventional nuclear medicine cannot reliably detect tumors of this size."
The two cancers missed by MBI were a small ductal carcinoma site and cancer within a patient who had extensive ductal carcinoma in situ throughout the entire breast. In her case, the cancer also went undiscovered by mammography and MRI.
The Mayo study also found that the recall rate for mammography was 9.2%, whereas MBI had a recall rate of 7.3%. Fifteen-month follow-up was completed with 341 patients.
The sensitivity of MBI was 86%, compared with 29% for mammography. Regarding specificity, MBI achieved 94%, compared with 91% for mammography.
Of 15 biopsies prompted by mammography in 2% of patients (15 of 762 patients), 20% were positive for cancer. Of 28 biopsies prompted by MBI in 3% of patients (26 of 762), 29% were positive for cancer.
Modality comparisons
In reviewing previous research on other breast imaging modalities, O'Connor noted that breast MRI has good sensitivity at approximately 80%, but specificity can vary from 50% to 80%, depending, in part, on whether the MRI breast screening is performed in a tertiary facility or a small community hospital. An MRI scan also can cost as much as 10 times the amount of a mammogram.
Scintimammography, which performs well with specificity, can have a loss of sensitivity in detecting increasingly smaller lesions.
While the American Cancer Society (ACS) recently recommended contrast-enhanced breast MRI as an adjunct to mammography in these women, O'Connor noted that variable specificity and high cost of MRI may limit its widespread use.
Cost estimates
Based on an estimated 1.5 million women in the U.S. who are at-risk for breast cancer annually and an average cost of $2,300 for an MRI scan, "you are looking at a $3 billion to $4.5 billion price tag for MRI, if it were to be an approved application in the U.S. Medicare does not reimburse for it," O'Connor said. "The cost of MBI is estimated at one-fifth to one-third the cost of MRI" and may decline as patents expire on sestamibi.
The one big drawback for molecular breast imaging, O'Connor noted, is the issue of radiation exposure. "Right now the radiation dose from 740 MBq of sestamibi is 6.7 mSv," he said. "One of the active research projects we have right now is to reduce the dose of sestamibi to somewhere between 70 and 100 MBq."
By Wayne Forrest
AuntMinnie.com staff writer
September 15, 2008
Related Reading
Solid-state scintimammography matches breast MRI, July 2, 2008
Breast gamma imaging spots DCIS better than mammo, MR, August 13, 2007
Solid-state dual-head camera supercharges molecular breast imaging, December 19, 2006
Molecular breast imaging sensitive for detecting smallest tumors, January 21, 2005
Copyright © 2008 AuntMinnie.com