PEBBLE BEACH, CA - Traditional image-guided therapy is giving way to a brave new world of therapeutic imaging. The difference is more than semantic, say scientists who are developing new technologies to heal patients as well as diagnose them. It amounts to a new emphasis on the cure, and myriad ways to achieve it with the aid of imaging technology.
Some techniques, such as focused ultrasound ablation, are using traditional imaging modalities in curative ways. Others, such as image-guided gene implantation, use imaging in ways that are more integral to the healing process than the traditional image-guided drainage and biopsy procedures. In any case, things are evolving fast, with hundreds of new technologies vying for attention.
"A variety of imaging techniques are now being used, and quite a few of them are also applicable to therapeutic applications," said Andreas Melzer, Ph.D., at the 2006 Society for Medical Innovation and Technology (SMIT) meeting on Thursday. He told of antitumor and vascular therapies, of depressed patients being treated with neurostimulation and neuroablation.
"Imaging has become such a dimension of diagnostics that it's now down to the molecular level, and allows us to image the interactions of drugs and different biological functions," said Melzer, who is from the Institute of Innovative Technologies and Management in Medicine (INSITE med.) at the University of Applied Sciences in Gelsenkirchen, Germany. Just around the corner are "laser-based medical photonics and also the use of imaging modalties for therapy such as photoporation and sonoporation," he said.
Photonic technology uses the properties of low-level laser light passing through tissue and blood. When these properties are correlated to physiological conditions, the process enables the detection of cancer via optical biopsy, analysis of hematology and blood gas, monitoring of hormonal cycles, and evaluation of burn wounds and other tissue damage.
Photoporation with a violet-diode laser can be used to introduce foreign DNA into living mammalian cells. Paterson and colleagues found that the beam perforated the cell plasma membrane to allow uptake of plasmid DNA containing an antibiotic-resistant gene.
Many advanced procedures are well-established, such as PET/CT following CT-guided liver ablation of hepatocellular carcinoma metastases. Overlaid precisely on the CT image, PET lights up if there are residual tumor cells (and unfortunately, sometimes even when there aren't residual tumor cells, Melzer noted).
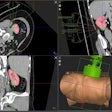
Intraoperative navigation is making more use of imaging that is incorporated dynamically into interventional procedures, rather than statically like earlier interventions. A surgical C-arm developed at Melzer's lab helps keep patients safer during surgery.
MRI is being primed for a bigger role in interventional procedures because it spares the patient a radiation dose, among other advantages. State-of-the-art MRI can image a beating heart, and in Germany, whole vascular body scans are being performed routinely in an hour. A brain study takes just 10 minutes; a heart or a colon takes 20 -- and 3D endoscopic MR colonography demonstrates excellent soft-tissue delineation.
"The question is who should be scanned by what age -- and what you do with all these data," Melzer said. And limitations in spatial resolution have proved challenging, he added.
Melzer said his group has worked with researchers at the German Cancer Research Center on an MR-compatible robotic system deployed inside a high-field MR scanner to deliver not only cannulas and catheters, but also targeted drugs. After the system moves the patient into position, it gets down to computer-aided surgery with augmented visualization of pathology.
MR-guided interventions are also aided by the development of so-called active MRI systems, which tag stents and other devices distinctively on MRI for easy identification, localization of intima, and even characterization of blood flow and potential thrombi.
An superelastic shape memory alloy discovered in the 1960s is being formed into an increasingly broad range of implantable medical devices, such as stents and filters. Nitinol is reasonably MRI-compatible, and exceedingly durable, according to recent animal and laboratory test results reported at the meeting.
Newly developed contrast agents based on ultrasmall iron oxide particles (USPIO) are an important aid to MR angiography, highlighting lymph nodes and vulnerable plaques based on their uptake by macrophages, Melzer said. High-field MRI offers three to four times the signal intensity of standard 1.5-tesla scanners, though much work remains to be done.
Ultrasound evolves
Thanks to recent developments, ultrasound is fast becoming a competitor to intraoperative MRI, Melzer said. Using "ultrasound fluoroscopy," H. Ermert and colleagues have shown the inside of a goldfish swimming and a child's hand flexing. The technique lacks the resolution of CT or MRI, but is a workable alternative for many applications, Melzer said. Three-dimensional ultrasound is also advancing rapidly.
Emerging therapeutic applications of ultrasound include sonoporation, and the activation of lysosomes and nanospheres with high-energy ultrasound. GE Healthcare of Chalfont St. Giles, U.K., and Tirat Carmel, Israel-based InSightec jointly developed the Exablate 2000 MRI-guided focused ultrasound surgery system.
The system marries high-field MRI for precise treatment planning, with focused ultrasound to heat and destroy tumors. The ultrasound heating is much faster and more focused than other ablation techniques, and has received U.S. Food and Drug Administration approval for the treatment of uterine fibroids, Melzer said, noting that many other lesion types, from bone metastases to liver, kidney, and prostate tumors, could potentially benefit from the technique.
Biomedicine
Another way to target a tumor for hyperthermal therapy is to have it absorb iron oxide-based nanoparticles before applying energy, which offers the advantages of precision -- and a deadly cellular "heat sink" effect when thermal energy is applied. Magnetic fluid hyperthermia is a minimally invasive cancer therapy that attacks cancers cells while leaving normal tissues largely unharmed.
Only the cancer cells absorb nano-sized iron particles, which are then subjected to an external alternating magnetic field, which heats and kills the cells containing the iron particles. The first clinical trials are set to be performed on brain tumor patients at Berlin's Charité Hospital.
Nanoparticles also have a bright future in imaging-specific display, selective binding and surface treatments, and drug transportation and delivery, Melzer said.
Researchers at the University of Cologne in Germany are experimenting with MRI-guided injection of stem cells into rat brains after iatrogenically induced infarction. The brain tissue at the site of the injection regrew and reorganized itself in the animal experiments, Melzer said.
Meanwhile, a self-assembling resonant target nanocube has been trained to scoop up targeted cells. Nanosphere activation has been successfully controlled by MRI. Nanoparticles have been directed to drill holes into cell nuclei, and are being used experimentally for molecular surgery.
"What I want to emphasize is that imaging is coming to a completely new horizon, combining medical technologies, drug delivery, and medical devices, with pharmaceutical and genetic functions, stem cells, and tissue engineering," Melzer said.
By Eric Barnes
AuntMinnie.com staff writer
May 12, 2006
Related Reading
PET, PET/CT help determine RFA outcomes in lung cancer treatment, May 12, 2006
IMRT to 4D radiotherapy rely on QA for accuracy, May 4, 2006
NEMA paper touts imaging's role in oncology, April 6, 2006
CARS suite of the future sees key role for image-guided intervention, June 23, 2005
Copyright © 2006 AuntMinnie.com