When it comes to upping the ante on radiation dose for non-small cell lung cancer (NSCLC), toxicity to the lungs and esophagus prevents a big payoff. But PET/CT has come up a winner for NSCLC radiotherapy planning, allowing European clinicians to escalate dosage without dealing a losing hand to normal tissue.
"Because FDG-PET has greater accuracy than CT for staging mediastinal lymph node areas of NSCLC, we hypothesized that only irradiating the nodal areas in the mediastinum that were positive on FDG-PET would be safe and beneficial," wrote Dr. Antoinet van Der Wel and colleagues in the International Journal of Radiation Oncology, Biology, and Physics (March 2005, Vol. 61:3, pp. 649-655).
Van Der Wel is from the Maastro Clinic at the University Hospital Maastricht in the Netherlands. Her co-investigators are from the hospital's departments of lung disease, radiology, and radiotherapy. Other authors are from University Hospital Aachen in Germany and the Gray Cancer Institute in Northwood, U.K.
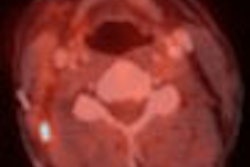
For this study, 21 patients with pathologically proven NSCLC underwent CT scanning (Somatom Plus, Siemens Medical Solutions, Erlangen, Germany) with 140 kV and 165 mA as the acquisition parameters. The CT scans were read by co-author Dr. Rob Lamers, Ph.D.
PET studies were performed within four weeks of CT on an ECAT Exact 922 scanner (Siemens/CTI Molecular Imaging, Knoxville, TN), one hour after the injection of 200-350 MBq of FDG. Co-author Dr. Michael Zimny read these scans.
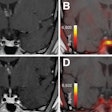
For radiotherapy planning, the gross tumor volume (GTV) and planning target volume (PTV) were defined using CT and PET/CT data. "Radiation dose escalation for the CT versus PET/CT PTV was calculated according to the constraints for the lung, esophagus, and spinal cord," the authors explained.
According to the results, the GTV of the mediastinal lymph nodes decreased from 13.7 cm3 on CT to 9.9 cm3 on PET/CT, with all dose-volume characteristics for the esophagus and lungs decreasing in favor of the combined modality. The volume of the esophagus receiving 45 Gy dipped from 45% to 34%; the volume of the esophagus receiving 55 Gy went from 30.6% to 21.9%. Finally, the volume of the lungs receiving 20 Gy fell from 24.9% to 22.3%.
"The dose could be increased from 56 Gy with CT planning to 71 Gy with PET planning.... The tumor control probability ... was estimated to increase from 14.2% to 22.8%," the authors stated. Among the 21 radiotherapy plans, 67% changed because of PET data, with radiation fields decreasing in 11 patients and increasing in three, they stated.
The group acknowledged that the study did have some limitations, including a lack of accounting for chest motion artifacts, which could have blurred the exact anatomic location of the lymph nodes. However, they pointed out that many PET/CT scanners automatically adjust for organ motion.
Controlled clinical trials are still necessary before PET/CT-based planning can become part of routine practice, the authors concluded, but stressed that their results suggest that PET/CT planning "may allow for intensive radiotherapy with or without concomitant chemotherapy, as well as a decrease in side effects."
By Shalmali Pal
AuntMinnie.com staff writer
March 16, 2005
Related Reading
PET/CT demonstrates staging strength over PET, CT, and PET plus CT, March 7, 2005
PET/CT hardware hybrid tops PET, software fusion for NSCLC staging, December 7, 2004
Copyright © 2005 AuntMinnie.com