At least one-fourth of patients who have pulmonary embolism (PE) don't undergo imaging tests other than chest radiography, despite recommendations for diagnosing the disease, according to a new study published in the April issue of the American Journal of Roentgenology.
It's a puzzling finding, said the researchers from the American College of Radiology (ACR) of Reston, VA, because a broad range of imaging tests are available. The findings may imply that despite concerns regarding the overutilization of medical imaging, there may be some diseases for which imaging is underutilized (AJR, April 2010, Vol. 194:4, pp. 1018-1026).
"It is noteworthy to find that in the diagnosis of PE, a condition for which both false-positive and false-negative diagnoses have serious consequences and for which reliable imaging tests are available, many patients apparently do not undergo imaging," wrote lead author and ACR research director Mythreyi Bhargavan, Ph.D., and colleagues.
The group used 2005 Medicare claims data, which included all insurance claims from physicians, hospital outpatient departments, and hospital inpatient departments for a random 5% sample of Medicare fee-for-service beneficiaries.
They identified patient characteristics such as age, sex, race, and cardiopulmonary conditions, as well as whether the patient lived in an urban or rural county. Bhargavan's team also identified geographic variations by state for the 10 most populous states, and the specialty of the physician who diagnosed the patient with PE. Site of care was categorized as the emergency department only, emergency department and inpatient, or inpatient only.
The researchers studied two groups from the data: patients who had symptoms that suggested PE and might have undergone testing for the disease, and patients with inpatient admission who had a definitive diagnosis of PE.
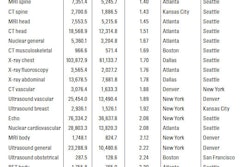
At least 63% of patients suspected to have PE underwent chest radiography. The most common other tests were:
- Echocardiography (26.7% of the study sample)
- Chest CT or CT angiography (10.7%)
- Cardiac perfusion (6.9%)
- Duplex ultrasound (7.3%)
For patients with an inpatient diagnosis of PE, about half underwent chest radiography. The most common other tests for this group were:
- Chest CT or CT angiography (49.1%)
- Duplex ultrasound (18.6%)
- Echocardiography (10.9%)
- Ventilation/perfusion scintigraphy (10.9%)
- Pulmonary perfusion only imaging (2.6%)
MRI or MR angiography of the chest was rarely used in either patient population, at 0.1%, the study found.
Workup variations
For the patients for whom PE was suspected, large variations were found in practice patterns among site of service, physician specialties, and geographic locations, according to Bhargavan and colleagues. But among patients with inpatient diagnoses of PE, there were fewer practice variations.
"We found substantial variation with respect to all the factors we investigated," they wrote. "Patients seen in more than one place of service tended to undergo more imaging tests than patients seen in only one place."
Among physician specialties, for patients with symptoms of PE, doctors tended to make heavy use of tests relevant to people with disorders treated by their specialty: Cardiologists tended to use echocardiography and perfusion imaging, while pulmonologists tended to use chest CT or CT angiography or duplex ultrasound.
This finding may show that physicians' choices of tests are determined by their specialties, whether or not the tests are appropriate, according to the authors.
"Patients whose condition was eventually diagnosed as PE and saw a cardiologist first were approximately two to three times as likely as patients whose first physician was not a cardiologist to undergo echocardiography or cardiac perfusion imaging," they wrote.
Geographic cures
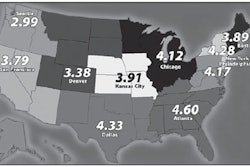
The team found substantial geographic variation in the use of imaging tests; for example, if other factors such as physician specialty and place of care were equal, patients in rural areas were less likely than those in urban environments to undergo echocardiography. Geographic differences probably reflect differences in physician practice patterns, according to the researchers: The differences found among patients who had PE were as dramatic as three to one in odds ratios, even after controlling for other variables.
The group measured state and regional differences in relation to California, the most populous state, and found that patients in most states and most regions had greater odds of undergoing each of the five tests than patients in California. Why? Perhaps because of the dominance of Kaiser Permanente in that state.
"Although we studied a fee-for-service population, the Kaiser Permanente HMO plays a particularly prominent role in healthcare in California," the authors wrote. "The research literature shows that, in general, where HMOs are prominent, their parsimonious care patterns spill over into the general practice patterns in the region."
The study's findings indicating that one-fourth of patients who had PE did not show evidence of having undergone imaging tests may have been influenced by the research focus on hospitals; in that setting, there is relatively little opportunity for physicians to overuse imaging via self-referral, Bhargavan and colleagues wrote. Or it could be that these patients were diagnosed before the dataset used for the study and appeared in the 2005 claims data because of a new problem.
In any case, the broad findings are probably reliable, according to the authors.
"Perhaps hidden by the outcry about overutilization is substantial underutilization for some clinical presentations," they wrote.
By Kate Madden Yee
AuntMinnie.com staff writer
March 31, 2010
Related Reading
DVT, pulmonary embolism common with superficial thrombosis, February 17, 2010
DVT predicts death in patients with pulmonary embolism, February 4, 2010
Survey: CT most popular choice for suspected PE, December 23, 2009
SPECT as accurate as CT for diagnosing pulmonary embolism, December 17, 2009
Copyright © 2010 AuntMinnie.com