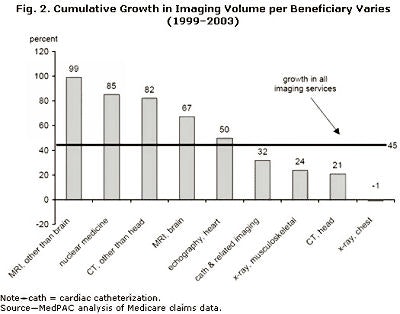

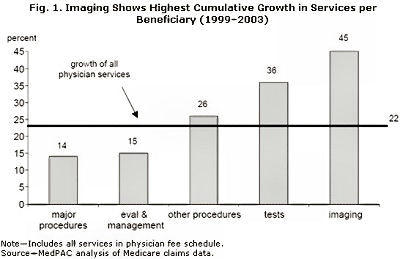
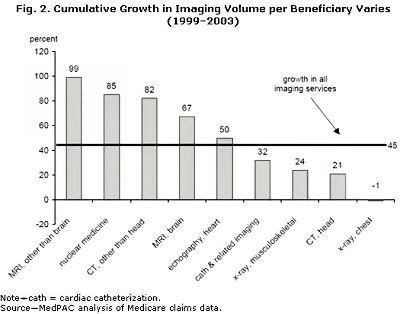
In MedPAC's recent "Report to Congress: Medicare Payment Policy" (March 2005), MedPAC has, once again, confirmed the fast rising rate of growth in imaging costs. In figure 1 below, we can see how imaging (inclusive of nonradiologist imaging) has been growing at rates even faster than the fast-growing nonimaging components of Medicare spending. Figure 2 demonstrates, just as dramatically, the rate of growth of the highest ticket items in our practices. While it becomes clear that cardiac imaging is a major driver, it is naive to infer that it is the sole reason for imaging cost increases.
 |
 |
MedPAC has begun a vigorous discussion on various ways to keep imaging costs down. They include the following:
Measuring physicians' use of imaging services
MedPAC has recommended that Medicare claims data be used to measure fee-for-service (FFS) physicians' resource utilization. MedPAC is recommending that the data be used to compare physicians with their peers in an effort to improve overall quality of care. MedPAC believes that providing the data has the potential to reduce service use. Since imaging accounts for much of the resource utilization, Medicare could eventually decide to provide incentives to physicians who decrease their imaging utilization. This is not explicitly considered at this time, but we should be wary. This could have a major impact on our practices, since nearly 90% of all Medicare beneficiaries fall into the fee-for-service group.
MedPAC is making this recommendation as part of the broader need to track clinicians' resource use. Radiologists' "modifications" to initial orders might also be tracked.
Expanding coding edits
This is a major and not unexpected approach for MedPAC to recommend. What is fortunate is that the agency has not gone so far as to use it on the professional component of our practices. MedPAC believes that certain practices are billing for more studies than are actually being performed (or, put another way, certain imaging procedures are correctly incorporated in certain codes and not separately billable examinations). In particular, MedPAC seems to feel that incremental examinations (a pelvic CT done at the same time as an abdominal CT) should not receive the full reimbursement as a standalone study. MedPAC is targeting the technical component only, in this instance.
Setting standards for physicians who interpret imaging studies
MedPAC's recommendation that standards should be set for physicians who bill Medicare for interpreting diagnostic imaging studies and that an independent private organization should administer the standards is very bold. It will likely be contested by many, but should be favorable for those of us concerned about encroachment on our practices, as long as we demonstrate that we are the standard-bearers.
Imposing standards for providers who perform imaging studies
MedPAC goes one step further in beginning to discuss who can provide the technical component of imaging studies. Some among our specialty will rightfully claim this is even bolder than the previous recommendation. MedPAC is explicitly discussing turf and self-referral, an area that Medicare has not really weighed in on before.
Enacting changes to the Stark laws
MedPAC has identified two areas of concern that it believes can be fixed in the current interpretation of the Stark laws (officially known as the Ethics in Patient Referrals Act). One area refers to the current exclusion of nuclear medicine facilities from the Stark laws. This exclusion would cease to exist if Congress follows MedPAC's recommendations. Further, MedPAC has taken aim at certain novel financial arrangements, as recently detailed in the Wall Street Journal ("MRI and CT Centers Offer Doctors Way to Profit on Scans," May 2, 2005; Page A1).
These arrangements allow for clinicians to profit from referring patients to certain MRI and CT facilities, by "leasing" slots, and thereby benefiting from the "in-office ancillary exception." Both of these changes can be beneficial to radiology practices, insofar as they limit true self-referral.
MedPAC decided that certain strategies cannot be recommended at the current time, despite their use in some private plans. Specifically, MedPAC did not weigh in on using preauthorization for imaging procedures. This is very fortunate, as the administrative costs of such a recommendation, combined with Medicare's relatively lower payment to begin with, would make provision of such services more difficult. MedPAC also has not recommended beneficiary education (because it is unproven, at this time) or the use of tiered networks (because there is a lack of data to suggest that cost-savings would accrue).
The MedPAC report also discusses other issues that either directly or indirectly affect our practice, including physician payment and pay-for-performance.
Physician services
MedPAC has recommended that Congress increase the conversion factor for physician services by approximately 2.7%. This is a decided change from the current congressionally authorized decrease (as per the sustainable growth rate legislation of the past decade) of nearly 5%. Congress must act on this to have an effect, but it would certainly be a welcome change from the current situation.
Pay-for-performance
MedPAC spends little time in its current report discussing physician pay-for-performance, but nonetheless makes a positive recommendation in this regard. How this is structured and whether it can be applied to imaging interpretation (particularly in the earlier rollout of such a plan) remains to be seen, but it is clearly on the horizon. Since the Centers for Medicare and Medicaid Services has already embraced pay-for-performance in hospital organizations and nursing facilities, we can expect a vigorous effort.
Overall, MedPAC's "Report to Congress: Medicare Payment Policy" is favorable to our specialty. MedPAC has been educated on many of the challenges that face cost-containment in U.S. medicine, and found that some of the solutions reside in our specialty. MedPAC clearly seeks intelligent outside advice on these matters. We need to be able to provide data and evidence that defend access to quality imaging.
By Dr. Howard P. Forman
AuntMinnie.com contributing writer
August 16, 2005
Dr. Howard Forman is an associate editor of health policy for the American Roentgen Ray Society (ARRS). This article originally appeared in the American Journal of Roentgenology (July 2005, Vol. 184:7). Reprinted by permission of the ARRS.
Related Reading
Medicare's condition in 2005: critical, June 15, 2005
Health benefits at work: what to expect in the future, May 24, 2005
National health expenditures and another year of 'unsustainable growth', May 4, 2005
ACC, ACR debate stats on imaging growth, April 18, 2005
ACR criteria cut imaging costs in Israel, January 11, 2005
Copyright © 2005 American Roentgen Ray Society