For the past few years, CT has been gathering force as a standalone modality for the integrated assessment of coronary heart disease -- a hefty task list that includes cardiac anatomy, function, perfusion, and viability. The techniques under investigation appear to work: The few studies comparing CT's performance for myocardial assessment to that of MRI have found roughly equivalent accuracy.
Now, using a second-generation dual-source CT (DSCT) scanner, U.S. researchers have added a trick they couldn't perform on their first-generation system -- dynamic evaluation of the time-resolved passage of contrast media through the myocardium.
In a proof-of-concept study published online this week in the Journal of Cardiovascular Computed Tomography, researchers from the Medical University of South Carolina in Charleston took advantage of the second-generation scanner's wider x-ray detectors to improve myocardial viability assessment at DSCT by, among other things, improving the assessment of microvascular obstruction in the myocardium.
Visualizing first-pass myocardial perfusion relies on time-resolved image acquisition during contrast administration, explained Dr. Gorka Bastarrika, Ph.D., and colleagues. Animal studies have shown feasibility and the potential for using the technique for both visual and semiquantitative assessment.
Myocardial assessment has remained suboptimal, however. High-quality time-resolved imaging studies in human subjects "will require greater volume along the z-axis of the heart combined with high temporal resolution if the effects of pharmaceutical stress on myocardial perfusion are to be evaluated," explained Bastarrika, Dr. Luis Ramos-Duran, Dr. U. Joseph Schoepf, and colleagues.
This advance was achieved with the introduction of broad-detector-array CT systems and second-generation dual-source CT; "however, these instruments have hitherto not been applied for the purpose of time-resolved myocardial perfusion imaging in actual patients with coronary heart disease," the authors wrote.
The study evaluated the feasibility of the group's protocol for integrative imaging of coronary heart disease in three patients referred for SPECT myocardial perfusion imaging for assessing coronary artery disease. All three subjects underwent stress perfusion and delayed-enhancement cardiac CT, as well as stress/rest perfusion and delayed-enhancement MRI.
Using a second-generation dual-source CT scanner (Somatom Definition Flash, Siemens Healthcare, Malvern, PA), imaging began with single-heartbeat CT calcium scoring at 2 x 128 x 0.6-mm sections, 280-msec gantry rotation time, 120-kV tube potential, and 73 mAs.
Next came prospectively triggered coronary CT angiography (CTA) after triphasic contrast injection, followed by a 70%-30% saline solution, all at 6 mL/sec. Prospectively triggered coronary CTA images were acquired at 2 x 128 x 0.6-mm sections, 280-msec gantry rotation time, 120-kV tube potential, and 320 mAs.
MRI and SPECT
Cardiac MRI studies were performed on a 1.5-tesla system (Magnetom Avanto, Siemens Healthcare) with stress perfusion MRI performed during peak adenosine stress using steady-state free-precession (SSFP, TrueFISP, Siemens Healthcare) perfusion sequences, followed by rest perfusion images 10 minutes later.
Rest and stress SPECT myocardial perfusion imaging was performed after intravenous administration of a technetium-99m radiopharmaceutical in a one-day protocol.
The researchers evaluated the perfusion imaging studies based on the 16-segment American Heart Association (AHA) model, interpreting SPECT and MRI images for fixed and reversible defects. They examined dynamic stress CT perfusion and MR studies in conjunction with delayed-enhancement CT and MRI viability scans.
Semiquantitative perfusion analysis was performed at CT and MRI with commercial software used to calculate the myocardial-to-left-ventricular upslope index, normalized to blood-pool intensity curves.
The results were encouraging: CT and MRI showed homogeneously perfused myocardium during adenosine stress that remained unenhanced on delayed images, indicating normal myocardium. Reversible ischemia was diagnosed when hypoperfusion visually lasted for more than six heartbeats under adenosine stress without enhancement on delayed scans. Myocardial perfusion defects were deemed fixed if hypoperfusion lasted for more than six heartbeats under stress and viability scans showed delayed enhancement.
Three cases
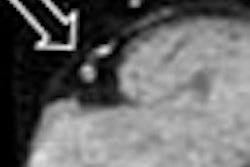
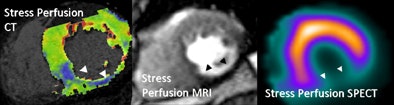
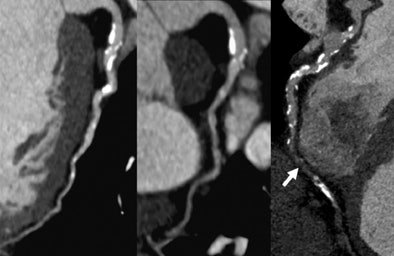
The following paragraphs describe three patients who underwent the comprehensive DSCT protocol along with SPECT myocardial perfusion and MRI for comparison. All images relate to the first patient.
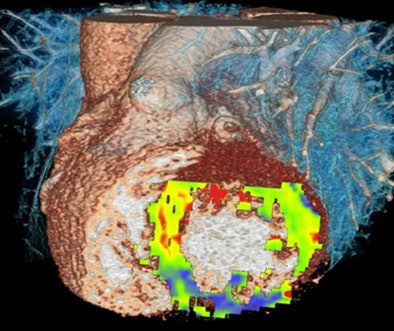 |
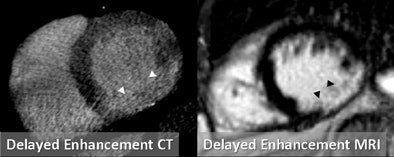
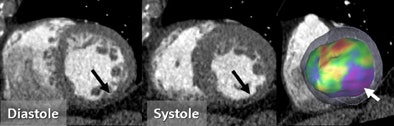
| Images are of a 64-year-old man with a past history of inferolateral myocardial infarction. Rest coronary CT angiography revealed distal right coronary artery occlusion. Functional analysis during systole and diastole showed inferolateral akinesis. First-pass adenosine stress dynamic perfusion CT demonstrated inferior and inferoseptal perfusion defect, confirmed on MRI and SPECT. This perfusion defect corresponds to chronic infarction, as confirmed by delayed-enhancement CT and MRI. Images courtesy of Dr. Gorka Bastarrika, Ph.D. |
 |
 |
 |
 |
The second patient was a 56-year-old man with a history of inferior myocardial infarction and right coronary artery angioplasty eight years earlier, presenting this time with recurrent atypical chest pain. Despite a history of remote myocardial infarction, stress/rest SPECT was deemed normal. Stress-perfusion and delayed-enhancement cardiac MRI showed preserved left ventricular function with chronic inferior subendocardial infarction.
Coronary CTA showed mild luminal irregularities in the right coronary artery, without significant obstructive disease. Stress first-pass myocardial perfusion imaging with CT revealed an inferior subendocardial perfusion defect, which was confirmed by MRI but not SPECT.
Regarding the third case, the patient was a 70-year-old man with a history of coronary artery bypass surgery (left internal mammary artery to left anterior descending coronary artery, radial arterial graft to circumflex coronary artery, and saphenous vein graft to distal right coronary artery) and prior right coronary artery stent placement. This time the patient was admitted for occasional chest pain.
Stress/rest SPECT showed anterior ischemia, while cine MRI revealed anterior and septal hypokinesis. Stress perfusion MRI showed perfusion defect of the anterior and septal midventricular segments. Coronary CT angiography demonstrated postcoronary artery bypass graft surgery status with patent grafts to the posterior descending artery and circumflex coronary artery, and occluded left internal mammary artery to left anterior descending coronary artery graft.
Stress first-pass SPECT with CT showed perfusion defect of the anterior and septal midventricular segments in agreement with stress MRI and SPECT studies. Total dose-length product (DLP) from all four cardiac CT studies including coronary CT angiography of the entire thorax was 1,463 mGy cm (calcium score, 24 mGy cm; coronary CT angiogram, 668 mGy cm; dynamic perfusion, 621 mGy cm; delayed acquisition, 150 mGy cm).
Only CT shows some infarcts
As shown in the cases above, the new technique "can demonstrate subendocardial infarction not seen on SPECT but confirmed by MRI, and can detect ischemia in good correlation with stress-perfusion MRI and SPECT," Bastarrika and colleagues wrote.
"We provide the first description of the technical feasibility of performing dynamic contrast-enhanced myocardial volume perfusion imaging with mechanical CT for detecting perfusion defects and myocardial infarction in patients with coronary heart disease," they wrote.
In the past, perfusion CT provided only a one-time static snapshot of the state of the myocardial blood supply during the time the respective portion of the myocardium was imaged, even when wide area detectors were used in the scanner, they noted.
When narrower area detectors are used, more cranial regions of the heart are imaged at a different perfusion phase than caudal regions, because contrast material continues to pass through during the longer CT acquisition -- thereby limiting the assessment of the hemodynamic significance of coronary artery stenosis on myocardial perfusion.
The study's limitations included the inclusion of just three patients, and radiation remains a concern, although the exposures were within the range of values described for conventional retrospectively gated CTA and equivalent to that of a thallium SPECT scan, the authors wrote. Thus, the contrast dose is substantial but remains lower than in some body applications.
Wider detectors would be helpful
Greater z-axis coverage with CT remains an important technological goal because the 73-mm coverage in the current technique requires substantial planning and careful patient positioning to avoid missing areas of the myocardium.
Based on stress CT imaging alone, it is impossible to differentiate between fixed and reversible perfusion defects; however, the differentiation of infarct and ischemia is enabled by the addition of delayed-enhancement CT and possibly by performance of prospectively triggered coronary CTA, "which may serve as a surrogate in lieu of a dedicated rest perfusion acquisition," they wrote.
The study shows the feasibility of the CT-based approach for integrative imaging of coronary heart disease, providing assessment of luminal integrity of the arteries, cardiac function, perfusion, and viability within a single modality, according to the authors.
"CT dynamic first-pass perfusion imaging performed with the technique introduced here combines high spatial and temporal resolution in a similar fashion as MRI, and may allow obtaining comparable results for estimation of myocardial perfusion," Bastarrika and colleagues concluded. "The tissue kinetics of iodine contrast agents and gadolinium chelates are similar. However, different from perfusion MRI using gadolinium-based contrast agents, there exists a linear relationship between myocardial contrast medium enhancement and iodine concentration, therefore potentially enabling the direct quantification of myocardial blood flow with CT."
The total radiation exposure from all three CT acquisitions is within the range of values described for a single, conventional, retrospective electrocardiogram-gated coronary CTA and is equivalent to thallium SPECT, Schoepf wrote in an e-mail.
By Eric Barnes
AuntMinnie.com staff writer
February 10, 2010
Related Reading
DECT cuts tests as a one-stop myocardial, coronary artery exam
Dual-source CTA turns in mixed results for coronary stenoses, July 30, 2009
Adenosine stress DECT equivalent to SPECT, MRI, November 21, 2008
Dual-source CT edges into cardiac SPECT turf, March 6, 2008
Study correlates CTA to angiography, myocardial perfusion SPECT, May 25, 2007
Copyright © 2010 AuntMinnie.com