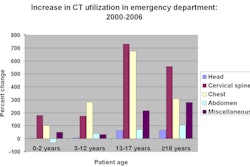
The development of dynamic volume imaging with 320-detector-row CT is opening new diagnostic and therapeutic windows to the brain, according to researchers at a high-volume imaging facility in Las Vegas.
With its wide 16 cm of anatomic coverage, 320-row CT scans the entire brain in a single gantry rotation, providing physiologic as well as anatomic information that cannot be obtained on conventional 64-slice scanners yielding a far-smaller 32 mm of coverage at a slice thickness of 0.5 mm.
Single-rotation volume acquisition is used to obtain unenhanced postcontrast head scans, while time-resolved 4D CT angiography (CTA) and CT perfusion scans are acquired in less than a minute using both intermittent and continuous scan elements.
Dynamic whole-brain coverage with 4D CTA adds the element of time, enabling precisely quantified perfusion evaluation that could pave the way to new diagnostic and prognostic applications.
At Nevada Imaging Center in Las Vegas, where the 320-row machine (AquilionOne, Toshiba America Medical Systems, Tustin, CA) was installed in April, dynamic volume CT has already been used for advanced neuroimaging in dozens of patients suffering from cerebrovascular disease, acute stroke, chronic cerebrovascular insufficiency, and occlusive disease.
Dynamic volume imaging of the brain "is one of the most exciting advances I've seen in my medical career, especially since most of my career has been spent as an interventional radiologist doing a lot of vascular procedures and a lot of neuroimaging procedures using catheter-based techniques," said Dr. William Orrison, chief of neuroradiology at Nevada Imaging Center and clinical professor at the University of Nevada School of Medicine in Las Vegas. "This is an incredible advance in terms of what we can look at without putting patients through the risk of a cath procedure."
A typical exam at Nevada Imaging Center, including noncontrast and contrast-enhanced dynamic volume CT, is performed with a single peripheral contrast injection of 60 cc Optiray (GE Healthcare Bio-Sciences, Buckinghamshire, U.K.) followed by 40 cc saline during the arterial phase and a reduced radiation dose, Orrison said.
Twenty-three intermittent volume datasets are acquired over 50 seconds, enabling the evaluation of arterial and venous information, dynamic blood flow assessment, and real-time review of the images, Orrison said at a Toshiba-sponsored advanced CT imaging symposium held earlier this month in San Francisco.
The protocol delivers routine contrast and noncontrast CT angiography, volume CT digital subtraction angiography, and full perfusion scanning. The aortic arch and carotid arteries can be added with about 10 cc additional contrast, increasing the scan time to about 67 seconds for the whole vascular tree, he said.
"You can obtain entire brain CT digital subtraction angiography (DSA) with real-time vascular flow as well as whole-brain perfusion," he said. "The CT DSA ... in many instances can replace routine DSA, resulting in a decrease in catheter DSA risk, lower radiation, and lower cost." The radiation dose is in the 4-6 mSv range -- about 7 mSv if the neck is included.
Orrison said that for about the same risk as a routine brain CT with and without contrast, 320-detector-row whole-brain perfusion scanning provides:
- Brain CT without and with contrast
- Routine CTA
- Real-time CT DSA with vascular flow
- Whole-brain perfusion including regional cerebral blood flow (rCBF), regional cerebral blood volume (rCBV), mean transit time, time to peak, and delayed blood-flow images.
Case studies
Presenting selected cases from his facility, Orrison said he was able to confirm or rule out disease in dozens of emergent-care patients, obtaining prognostic information in some and evaluating treatment response in others.
For example, in 320-detector-row CTA imaging of a 32-year-old man complaining only of decreased vision, the presence of dramatically increased perfusion indicated a "huge meningioma" frontally, Orrison said. The patient's symptoms resolved after a successful operation.
But most cases involve hypoperfusion, Orrison said. In a 77-year-old asymptomatic woman, for example, an internist had noticed a fairly loud carotid bruit in the course of a physical exam. Follow-up ultrasound showed a fairly low-grade stenosis, but MRI results indicated a significant blockage.
 |
| CT of a 77-year old asymptomatic woman with a carotid bruit reveals severe (85%) stenosis of the left carotid artery (above). However, brain perfusion maps (below) demonstrate normal regional cerebral blood volume (rCBV, left column), regional cerebral blood flow (rCBF, middle column), and mean transit time (MTT, right column) in axial, coronal, and sagittal planes (top, middle, and bottom rows, respectively). The results suggest that autoregulation of cerebral blood flow has successfully compensated for the stenosis. |
 |
"Now she has conflicting reports, so they sent her to us for evaluation," he said. "We found that she did indeed have about 85% stenosis of her left carotid artery [at CT]. She wasn't sure what to do with this, and went to several prominent internists. Some thought she should have it operated on, some were recommending aspirin therapy, so she came back to ask our opinion."
Orrison said his major concern was evaluating blood flow to the cranium in light of the stenosis. Standard 320-detector-row CTA with digital subtraction showed normal blood flow, as did perfusion imaging. Brain perfusion on the bruit side (left) was actually slightly better than the right. It appeared that the patient had more than adequately autoregulated the flow to compensate for the 85% carotid stenosis, he said.
"There was no deficit in her brain at all, and no arterial perfusion deficit, so she's getting an aspirin a day and nothing else," Orrison said. "And I think everyone who's taken care of her is now comfortable about how to proceed."
|
|
| A 42-year-old woman who presented for evaluation of possible cerebral aneurysm was imaged on the 320-detector-row scanner, and had 4D (3D volume over time) CT digital subtraction angiography reconstructions performed demonstrating normal intracranial vascular anatomy. Video courtesy of Dr. William Orrison. |
| Having trouble viewing this clip? Click here to download the free Flash player. |
The situation was less promising in a 45-year-old man with headaches and a presumptive diagnosis of vasculitis. Decreased vertebral artery flow due to stenosis was seen in the "string of beads" appearance of the stenosed vessel. Perfusion imaging showed near-normal flow in the brain stem but significantly decreased perfusion in the frontal lobes with "vastly decreased basilar artery perfusion," Orrison said.
"What I think is going on here is that the brain stem has a lot more demand for blood flow than the frontal lobes -- basically breathing is a lot more important than thinking," Orrison said. "I think basically what we have is a ... 'steal' phenomenon where the brain says we're going to keep breathing no matter what and think later."
 |
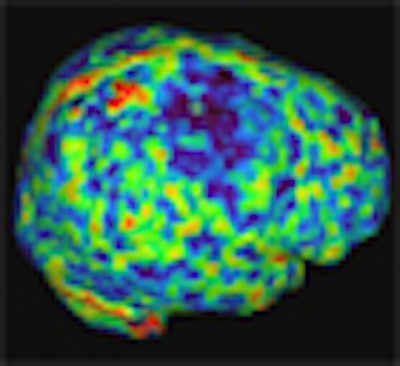
| In a 45-year-old man with vasculitis, 320-detector-row perfusion CT (PCT) shows perfusion deficits as focal decrease in regional cerebral blood volume (rCBV, above), regional cerebral blood flow (rCBF, below) and mean transit time (MTT, bottom) in the right superficial posterior frontal cortex. All images courtesy of Dr. William Orrison. |
 |
 |
Similarly, a 71-year-old man had a high-grade stenosis of the basilar and distal vertebral arteries at CT. Despite these findings, perfusion remained near normal in the posterior brain, with perfusion deficits primarily in the frontal lobes, suggesting another potential case of steal phenomenon, Orrison said.
CT with DSA reconstructions is particularly useful for evaluating patients who have undergone coil embolization of aneurysms, Orrison said. "In real-time you can see the coil in different planes, and some residual aneurysm, but there's no abnormal venous flow," he said of one case. The DSA reconstructions subtract out the coil and bone nicely, eliminating the need to follow up with invasive angiography, he said. Perfusion CT confirmed normal blood flow throughout the brain.
"This is probably the modality of choice for patients who have had aneurysms and prior embolizations and aneurysm clipping, because we don't have to put them through standard angiography and I think we can get excellent follow-up exams," Orrison said.
|
Having trouble viewing this clip? Click here to download the free Flash player. |
Changing habits to prevent stroke
One patient with failing eyesight and multiple poor lifestyle habits was warned after CT that a stroke was imminent. The patient, a 41-year-old overweight smoker with diabetes, was referred for evaluation after his ophthalmologist was no longer able to adjust the patient's eyeglass prescription to normal vision. CT perfusion revealed bilateral perfusion deficit of the occipital cortices.
"He had a significant flow defect exactly where you'd expect to see it for his clinical symptoms," Orrison said. "I brought him in and said, 'I will show you exactly where your stroke is going to occur if you don't do something.'"
Thus motivated, the patient returned a few months later having quit smoking, gone on a diet, and initiated a strict control regimen for his diabetes.
Another patient presented with severe headaches and a history of vasculitis. Was it recurring? Segmental CTA revealed an irregular internal carotid artery with a string of beads pattern demonstrating impaired blood flow. CT perfusion imaging confirmed the vasculitis and showed the area of impending infarction. After two weeks of steroid therapy the patient was rescanned; brain perfusion had returned to normal.
"What we've shown is that it is indeed possible for us to take images of areas at risk of infarction and reverse that, and we can normalize people," Orrison said. "I think we can identify areas of perfusion that are quite different than we thought they might have been with this technology. And I think we have a better tool for assessing any type of small vessel disease that we may see in these individuals."
A 71-year-old woman with persistent headache was referred to the facility after outside evaluation was deemed inconclusive. She underwent a routine 320-detector-row CT angiography with DSA reconstructions and perfusion imaging, which revealed drastically delayed perfusion. The surface volume of the angiogram showed a large area of hypoperfusion.
"The patient was very aggressively managed on her antihypertensive medications, and we ... recommended to her physicians that they may want to back off a little on that management," he said. "She may actually need the extra blood flow to her brain. That's one of the things we've noticed in a lot of patients we're evaluating. Many are very aggressively managed, even symptomatic on their antihypertensive medications, and we find these perfusion deficits."
A 56-year-old man underwent an elective facelift procedure and developed severe neurological deficits later that evening. Perfusion imaging showed a severe cerebral infarction. But after undergoing 22 hyperbaric treatments over three months, the patient's clinical condition had improved dramatically. Follow-up 320-row CT perfusion imaging three months later showed markedly improved perfusion.
Based on the initial promising results, the patient is now undergoing a regimen of 90 hyperbaric treatments over 12 months and will be scanned again as he completes the next 68 treatments, Orrison said.
In short, 320-row technology is providing an opportunity to "measure things we couldn't measure before, to make diagnoses we couldn't make before, and to look at opportunities to treat people and look at results of those treatments," Orrison said.
The technology is having an unexpectedly important impact on patients before, during, and after they infarct, enabling physicians to monitor more aggressive therapies, he said. It has an obvious application for patients who present to the emergency department with an acute infarct, though clinical studies are needed to validate the emerging applications.
"You can immediately get a CT with and without contrast, you can get a cerebral angiogram, and you can get a detailed perfusion scan in less than 60 seconds,"
he said. "So it's clear in that setting that it's going to have a pretty dramatic effect on patients."
"This high-yield low-risk brain evaluation provides new information for the assessment of neurovascular disease, has an obvious role in stroke detection, and a potential role in prevention and treatment that for me is very exciting, and I think there's a lot more to come," Orrison said. "I think it's a fantastic tool for us to help patients in the future."
By Eric Barnes
AuntMinnie.com staff writer
October 20, 2008
Related Reading
Flexibility of 320-slice CT boosts cardiac imaging options, October 3, 2008
Thrombolysis benefits stroke patients with fluctuating neurologic picture, September 5, 2008
Tenecteplase faster, more effective at cerebral artery recanalization than tPA, February 27, 2008
Part II: Modalities, input, and image processing see stroke differently, March 3, 2008
Part I: Stroke imaging hones in on preventable infarction, February 21, 2008
Copyright © 2008 AuntMinnie.com