LAS VEGAS - Finding ways to handle rising concerns over radiation dose from CT scanning was the subject of a series of presentations Tuesday at Stanford University's International Symposium on Multidetector-Row CT. While several of CT's leading experts expressed frustration about the level of misinformation in the lay press on radiation dose, they acknowledged that more needs to be done to reduce dose to the lowest possible levels.
Radiology experienced a "perfect storm" of increased public concern about radiation at the same time that new generations of more powerful scanners are delivering more dose. The average dose delivered to patients from medical radiation has grown significantly since the 1980s, when the annual average per capita radiation dose from medical procedures was 0.54 mSv; today, that number stands at 3.2 mSv, according to Dr. James Brink of Yale University in New Haven, CT.
CT is obviously a major driver of increased dose. Some 67 million CT scans were performed in the U.S. in 2006, representing about 12% of the total studies using ionizing radiation, but CT contributes 46% of the collective annual dose received by U.S. patients.
In addition, rising radiation dose has been the topic of a number of papers published in prestigious academic journals highlighting the risks of medical radiation, specifically radiation delivered by CT. The New England Journal of Medicine (NEJM) in November 2007 published a study that claimed that one-third of CT scans were "medically unnecessary," while a study in the Journal of the American Medical Association (JAMA) in July 2007 found that certain patient groups had a 1 in 114 chance of developing cancer in their lifetime due to radiation exposure from coronary CT angiography studies.
There are signs that the bad press is starting to have an impact. Several major academic institutions have reported falling CT procedure volumes in the last four to five months, Brink said, including Yale. An even higher number of imaging facilities are reporting anecdotal stories in which patients are refusing to undergo CT exams or are asking for alternative modalities.
More light than heat?
But to what extent do the public and referring physicians really understand the relationship between CT radiation dose and medically induced cancer? And is the radiology community starting to take their concerns seriously?
Unfortunately, the risk of developing cancer from a medical procedure such as CT is very real, according to Cynthia McCollough, Ph.D., from the Mayo Clinic in Rochester, MN. But there is much disagreement over the relationship between radiation dose and cancer at levels below 100 mSv, where CT procedures typically fall, she said.
Much of the data on radiation dose and cancer is based on studies of atomic bomb survivors, who received far higher radiation doses than today's average CT patient. But, absent any other evidence to the contrary, most radiation experts have settled on the linear no-threshold theory, which states that radiation still has a carcinogenic effect regardless of the dose level.
Based on reports from the Committee on the Biological Effects of Ionizing Radiation (BEIR) analyzing A-bomb survivor data, experts have settled on a ratio in which there are five cancer deaths per 100,000 population per mGy of dose delivered. Based on these estimates, CT is responsible for a 0.05% increase in cancer, McCollough said.
But a number of recent academic studies, such as the NEJM and JAMA articles, have taken established figures on radiation dose and cancer risk and applied them in ways that don't reflect the way CT is really used, according to Dr. Joseph Schoepf of the Medical University of South Carolina in Charleston.
For example, the July 2007 JAMA paper found that certain patient groups had a 1 in 114 chance of developing cancer after a cardiac CT angiography. However, this figure applied only to 20-year-old women, few of whom are receiving cardiac studies, Schoepf said.
Schoepf's institution conducted its own study along the lines of the JAMA research to see for themselves what the risk was in a more realistic clinical environment. They conducted cardiac CT studies with a 64-slice scanner (Sensation 64, Siemens Healthcare, Malvern, PA) on 104 patients (64 men, 40 women) with a mean age of 59 years.
In this group of patients, radiation doses were highest in radiosensitive organs such as the breast, at 89 mGy, and the lungs, at 79 mGy. The BEIR data indicate that this should result in an increased risk of cancer mortality of around 1 in 1,000, and 1 in 500 for certain patient groups more sensitive to radiation dose, such as women and those who are younger and lighter. When you consider the long latency period of cancer, in some cases as long as 30 years, it's easy to conclude that many patients will not live long enough to develop medically induced cancers.
"Even if you look at the most vulnerable patients, the cancer risk is at most double that of average patients, so overall, the radiation risk to the typical clinical patient population that undergoes cardiac CT is significantly lower than what has been flaunted by the lay press for radiation risk from cardiac CT," Schoepf said.
New technologies
Several presenters during the discussion talked about new technologies under development that could reduce radiation dose even further. Dr. Michael McNitt-Gray of the University of California, Los Angeles, reported on using a dose-modulation technique (CareDose 4D, Siemens) to reduce the dose delivered to breast tissue in women receiving CT scans. They found that the technique reduced dose by an average of 32%, from a median dose of 22 mGy without the technique to 13 mGy with it. Dose savings were typically greater with larger patients than smaller ones, McNitt-Gray said.
Norbert Pelc, Sc.D., from Stanford discussed the development of a prototype scanner using what he called an inverse-geometry CT (IGCT) architecture, which Stanford is working on in collaboration with GE Healthcare of Chalfont St. Giles, U.K. Rather than employ a larger number of detector rows, the system uses an array of three rows of x-ray sources, each with 12 focal spots, that rotate around a relatively small detector array. The x-ray sources are turned on and off depending on the type of patient and organ that's being studied, potentially giving users unprecedented control over dose. Experiments with the system indicate that it can produce images with very low dose and image noise, Pelc said.
Education is needed
Most of the presenters concluded that even though much of the information appearing in the lay press either overstates or misinterprets the risk of developing cancer from CT scans, the risk is significant enough to warrant the attention of radiologists. And ironically, many radiology professionals themselves still underestimate the risk of developing cancer from CT.
Brink discussed how Yale started a program to monitor dose by having technologists record the dose length product (DLP) for exams, which is available on any CT scanner. The DLP can be multiplied by an organ-based conversion factor, such as 0.17 for the chest, abdomen, and pelvis, to calculate the dose received by the patient. Otherwise, RTs and radiologists simply aren't aware of the dose being delivered during CT studies.
Other techniques include color-coded guidelines that make it easier for technologists to set imaging parameters for pediatric patients of different sizes or placing radiation alert notices on the film jackets of patients who are at risk of CT overuse, such as younger patients with benign diseases who have received more than five scans, or those who have received more than 100 mSv of cumulative radiation exposure.
Meanwhile, the Image Gently campaign, launched in January 2008 by 13 radiology-related organizations, aims to provide awareness and education regarding pediatric radiation dose. Participating in the American College of Radiology (ACR) CT accreditation program can also help facilities learn more about reducing dose, Brink said.
Such efforts can be successful, Brink believes. He pointed to initiatives in Europe that are probably the reason why the average annual cumulative exposure to medical radiation for Europeans falls in a range of 0.7 to 2.0 mSv, compared to 3.2 mSv in the U.S. "I think our European colleagues are 10 to 15 years ahead of us," Brink said.
But cutting back on CT usage can have a downside, as pointed out by one attendee from Europe in the audience.
"It sounds funny from the German perspective because we have been very sensitive to radiation, but we have more lawsuits recently from not having performed a CT scan than from performing a CT scan with radiation," he said.
By Brian Casey
AuntMinnie.com staff writer
May 15, 2008
Related Reading
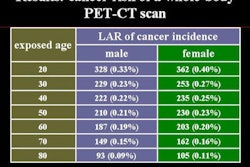
Study evaluates radiation dose, cancer risk for whole-body PET/CT, May 9, 2008
Researchers recommend alternatives to CT, April 15, 2008
ACC news: CTA dose varies widely, could be lower, April 2, 2008
Prospective gating drops cardiac CT radiation dose, March 10, 2008
New studies examine CR, CT radiation dose, March 9, 2008
Copyright © 2008 AuntMinnie.com