CHICAGO - Patients who take oral anticoagulants may risk developing significant coronary and aortic calcification. In a study that casts a wary eye on the routine use of the vitamin K antagonists such as warfarin, researchers from Aachen, Germany, found that long-term oral anticoagulant therapy was independently associated with increased calcium scores and valvular calcium deposits.
To date the evidence linking oral anticoagulation (OAC) therapy with increased calcification has been insufficient, said Dr. Andreas Mahnken in a presentation Friday at the 2005 RSNA meeting.
Vitamin K antagonists are known to affect the synthesis of the matrix Gla protein, which inhibits calcification in tissues, said Mahnken, who is from the Aachen University of Technology.
"We know there might be a correlation between the severity of coronary artery calcium and the presence of matrix Gla protein, reported about a year ago," he said (Jono S. Journal of Thrombosis and Haemostasis, 2004, Vol. 91, pp. 790; Schurges LJ. Blood, 2004, Vol. 104, pp. 323). "We also know that calcification is usually greater in patients who use oral anticoagulants for a long time, but we don't know what's going on in patients who have aortic stenosis."
The researchers sought to determine if there is an association between the use of oral anticoagulants and Agatston calcium scores, as well as aortic calcification.
Their prospective study examined 86 patients with aortic stenosis (53 men, 33 women; mean age 71 ± eight years) including 23 on long-term oral anticoagulant therapy (OAC) for six to 384 months (mean 88 months ± 113). Those with diseases associated with increased coronary calcification, such as Paget's disease, hyperthyroidism, and elevated serum calcium were excluded.
Most patients were on anticoagulant therapy for chronic atrial fibrillation (n = 16, 70%); other indications included low ejection fraction due to nonischemic cardiomyopathy (n = 3, 13%), recurrent deep venous thrombosis (n = 2, 9%), and recurrent PE or stroke (for each indication n = 1, 4%).
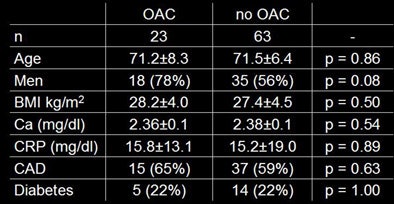 |
| Patient profiles were very similar for the 23 patients on OAC compared to the 63 non-OAC patients. Chart courtesy of Dr. Andreas Mahnken. |
All patients underwent MDCT imaging on a 16-row scanner (Sensation 16, Siemens Medical Solutions, Erlangen, Germany) at 12 x 0.75 mm, 120 kVp, 133 effective mAs, and 3-mm slice thickness with 2-mm overlapping reconstructions. The images were evaluated for Agatston coronary calcium score and same scoring method was used for aortic calcification, Mahnken said. Echocardiography was also performed to assess the presence of stenosis.
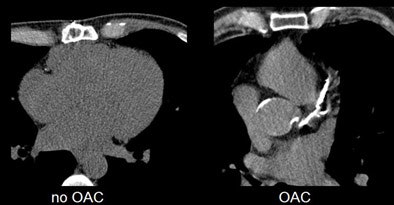 |
| Compared to non-OAC patient with aortic stenosis (left), typical OAC patient (right) shows extensive aortic and coronary calcium burden. Images courtesy of Dr. Andreas Mahnken. |
The results showed significant differences in coronary calcium burden between the two patient groups. The mean coronary calcium score in patients without OAC was 738 ± 978 versus 1,561 ± 1,141 in patients with long-term OAC (p = 0.024). Similarly, the mean aortic calcium score was 1,070 ± 1,085 in patients without OAC versus 2,410 ± 1,759 in patients with long-term OAC (p = 0.002).
"There was no correlation between the duration of the oral anticoagulation therapy and the coronary (p=0.35) or aortic calcification score (p=0.31), but it's important to note that we only included patients … with at least 6 months of anticoagulation therapy," Mahnken said.
Multiple linear regression analysis found that OAC was an independent predictor of coronary calcium score (p = 0.011 for OAC, compared to p = 0.045 for male gender, p = 0.049 for hypertension).
"We conclude from our findings that oral anticoagulation is associated with increasing levels of calcium in the coronary arteries as well as aortic valve, " Mahnken said. "This is due to the decreased protection against tissue calcification which is caused by the decreased vitamin K activation of the matrix Gla protein," he said. "This will be of clinical interest in patients who have aortic stenosis, and we expect them to have a faster increase in the calcification level."
The effect will need to be confirmed in larger trials; the group has initiated a five-year study that is already under way, he said.
"We are sure that we are also exposing young patients to a higher risk of developing vascular calcification," Mahnken said in response to an audience member who asked about the age distribution of increased calcification. The department of nephrology at his institution has come to the same conclusion, he said.
"Everywhere in Europe there is heavy discussion of this issue, because all patients undergoing dialysis, for example, have problems with oral anticoagulation," he said, adding that warfarin is strongly implicated in the development of calcification that is independent of the calcification risk of dialysis alone.
Internal medicine doctors and pathologists really became aware of the problem with OAC about a year ago, and the interest has intensified since that time, Mahnken told AuntMinnie.com. "But it takes a long time before radiologists become aware of it because we are farther away from the patient," he said.
By Eric Barnes
AuntMinnie.com staff writer
December 2, 2005
Related Reading
Caution: U.S.A. may be hazardous to your health, October 3, 2005
Coronary calcium screening seen useful beginning between age 40 and 50, September 23, 2005
Low-dose CT calcium scores near-equivalent of higher dose, September 20, 2005
CT coronary calcium results vary by scanner, body type, May 31, 2005
Radiologists correlate coronary calcium with other CVD markers, April 6, 2004
Copyright © 2005 AuntMinnie.com