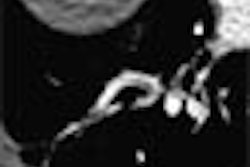
Investigators in Germany used contrast-enhanced multidetector-row CT to quantitatively assess noncalcified coronary plaque. They found that the exam had predictive value for detecting some cases of coronary artery disease that would have gone undetected using traditional CT calcium screening methods.
"(CT) has become an established method for noninvasive and highly sensitive detection of coronary artery calcifications, wrote Dr. Konstantin Nikolaou and colleagues in European Radiology. "Yet calcified plaques are probably the result of repetitive plaque rupture and healing, causing shrinkage of the lumen vessel with subsequent stenosis. Earlier stages of atherosclerosis without calcifications might be more prone to rupture, resulting in acute cardiac events." (European Radiology, online edition, August 20, 2003).
The team, from the University of Munich in Germany, sought to assess the incidence of noncalcified plaques in MDCT, and also determine the predictive value of the vessel wall changes in assessing coronary artery disease. Then they used a volumetric imaging to further illustrate the plaque burden detected by the exam.
The group examined 179 patients (123 men, 56 women, ages 61 ± 12 years) at high risk of coronary artery disease. Before undergoing both a CT calcium scan and contrast-enhanced MDCT angiography, all of the patients had also undergone catheter coronary angiography within the preceding 10 days.
The subjects underwent calcium screening on a four-detector CT scanner (Somatom Sensation 4, Siemens Medical Solutions, Forchheim, Germany) with collimation of 4 x 2.5 mm, 80 kVp, 300 mAs, and 3-mm slice reconstructions with 1.5 mm overlap.
They were then given 120 ml of non-ionic contrast material (300 mg iodine, Solutrast 300, Schering, Germany) at a flow rate of 3 ml/s. MDCT angiography was performed on the same scanner using 4 x 10 mm collimation, 0.5 sec rotation time, 120 kVp, 400 mAs, with a scan time of 35 to 40 seconds required to cover the heart. Data were reconstructed with contiguous 1.25 mm thick images at increments of 0.7 mm, the authors wrote.
Calcified plaque was assessed on the scanner's standard postprocessing workstation using commercial calcium screening software (Siemens Wizard), and a threshold of 130 HU to determine the Agatston score, volume equivalent and total calcium mass.
For interpretation, plaque was divided into three types: calcified plaques, mixed plaques and non-calcified plaques, with quantification performed only in the 53 patients who presented with true noncalcified plaques. The arteries were analyzed for both calcified and noncalcified plaque, using the axial slices and thin-sliding MIPS. The mixed plaques were assessed manually as the sum of calcified and non-calcified plaques, and the results analyzed by means of correlation and regression coefficients, the authors wrote.
According to the results of both calcium screening and contrast-enhanced MDCT angiography, 73% (131/179) of patients showed calcified or mixed plaques, and 27% had no detectable plaques. Purely noncalcified plaques were found in 30% (53/179) patients, "mostly together with calcified or mixed plaques at other sites of the coronary artery tree." In 41 patients there was no evidence of CAD).
Fifteen percent (7/48) of the patients with negative a calcium scan were found to have noncalcified plaques on noncontrast CT. And catheter angiography showed significant stenoses (> 75%) in three of the 7 patients. (The other cases included minor wall irregularities found in 2 patients, and normal lumen on catheter angiography in 2.)
For statistical analysis, the group performed an unpaired Wilcoxon test that considered the number of calcified, mixed and noncalcified plaques, and their relation to the severity grade of coronary artery disease.
"The mean number of calcified plaques increased significantly from grade 1 (n=6) and 2 (n=8) to grade 3 (n=39) whereas the mean number of mixed and noncalcified plaques did not increase (significantly) depending on the severity of CAD," they wrote. (Grades 1 and 2 were combined for statistical analysis due to the small numbers of each.)
Wilcoxon analysis of the quantitative values of calcifications measured by Agatston score, volume and mass showed that all three measures increased significantly from grades 1 and 2 to grade 3. As for risk factors, statistical analysis using a Chi-square test showed that hyperlipidemia was the only factor that showed a statistically significant increase in patients with calcified, mixed and noncalcified plaques (p=0.0265).
"The density of these non-calcified lesions has been reported by independent groups and in various vascular territories to be between 0 and 130 Hounsfield Units, (depending on) the content of lipid and fibrotic tissue as proven by histopathology or intravascular ultrasound," the authors wrote. "...The high standard deviations found may be due to the variety of tissue components combined in a single voxel. Therefore, a reliable differentiation of fibrotic and lipid-rich plaques may not be possible using MDCT, due to an overlap of the densities measured and the complexity of the lesions."
To gauge the predictive value of non-calcified plaques, the authors reported that the 7 patients who had negative CT calcium scans but positive MDCT angiography showed an overall higher risk factor profile, "...with a higher percentage of nicotine abuse (83%), obsesity (67%), hypertension (67%) and diabetes (50%)" than the 179-patient cohort as a whole, for whom the same percentages were 46%, 28%, 55% and 21%, respectively, they wrote.
Limited spatial resolution was cited as the principal limitation of the technique that prevented precise measurements of plaque volume and composition. This can be expected to diminish as the number of detectors increases, however.
While intravascular ultrasound has been found to be useful for the depiction of the coronary artery wall, it is invasive, and therefore unsuitable for a screening population, the authors wrote. MDCT angiography offers the advantage of being noninvasive, though it comes with a radiation dose.
"(MDCT) screening of these vessel wall changes will identify some patients with manifestations of CAD that would be missed in a calcium screening test," they concluded. "Thus, in selected patients groups with characteristic risk factor profiles, an additional contrast-enhanced study should be performed."
They added that future studies should address the reproducibility of the quantitative measurements, and clinical outcomes in patients with noncalcified plaques.
By Eric BarnesAuntMinnie.com staff writer
September 24, 2003
Related Reading
Calcium-scoring methods study says it's all good, September 10, 2003
Coronary calcium scan gains ground as prognostic tool, August 6, 2003
Study finds blacks have less coronary calcium than whites, February 17, 2003
Thin-collimation MDCT identifies more coronary calcium, December 18, 2002
Population-based study links coronary calcium and mortality, December 1, 2002
Technology keeps CT vital for coronary assessment, November 13, 2002
Copyright © 2003 AuntMinnie.com