The ability to scan a wider variety of patients -- and to do it quickly, with less contrast and far fewer artifacts -- is an important advantage of 320-detector-row CT, according to a cardiologist who has been working with the scanner since it was installed earlier this year.
In fact, Dr. Tony DeFrance, an associate professor of medicine at Stanford University in Stanford, CA, and chief of cardiac imaging at the Nevada Imaging Center in Las Vegas, sees a bright future for cardiac CT on all scanners, owing to the modality's increasingly demonstrated capabilities in the detection and diagnosis of cardiac disease faster and more cost-effectively than other methods.
The coming shift to CT certainly won't please every stakeholder in the healthcare system, he added, but the results to date ensure that it will proceed.
DeFrance spoke earlier this month at a San Francisco CT imaging symposium sponsored by Toshiba America Medical Systems of Tustin, CA, the manufacturer of the 320-detector-row AquilionOne system.
DeFrance, who has scanned about 250 patients with suspected heart disease since the machine was installed this spring at Nevada Imaging, cautioned that some of his early impressions of the scanner, based on six months of clinical use, have yet to translate into published studies.
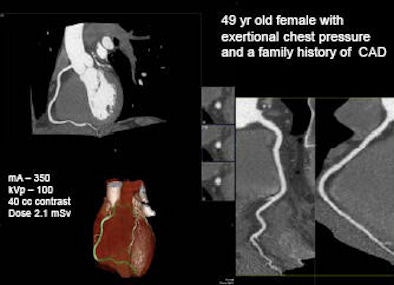 |
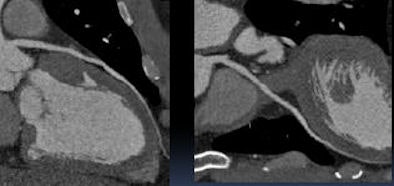
| In a 49-year-old woman with exertional chest pressure and a family history of coronary artery disease, prospectively gated 320-slice CT angiography ruled out coronary artery disease with a radiation dose of 2.1 mSv. All images except one noted below are courtesy of Dr. Tony DeFrance. |
The biggest advantage of 320-detector-row dynamic volume CT scanning is its 16-cm anatomic coverage that can scan the heart in a single beat, eliminating misregistration artifacts and enabling lower dose imaging compared to 64-slice scanning, DeFrance said. The scanner features 320 x 0.5-mm detector elements and a 350 msec rotation time.
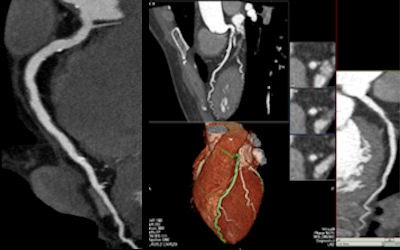 |
| A 44-year-old man with atypical chest pain and a family history of coronary artery disease. Far left, 320-slice coronary CT angiography was performed from the emergency department. Patient has mild mixed plaque in the right coronary artery. Right, same patient showing mild noncalcified plaque in the left anterior descending artery. |
"With 64-slice CT we get about 3 cm [of anatomic coverage] per rotation, so it takes six to eight heartbeats" to scan a heart, he said. "Contrast that with 320-slice, where we can capture an image in a fraction of a heartbeat." In turn, he said, the ultrafast acquisition solves a lot of other problems that have limited coronary CT angiography (CTA) to date.
First, DeFrance said, single-beat scanning eliminates misregistration, the most common type of artifact.
"You're counting on the heart being in the same place for each beat, and when that doesn't happen it's called misregistration," he said. "Because the 320 is a single snapshot, there are no more changes in contrast [opacity] from beat to beat, and there are less artifacts from stents and calcium."
 |
| With one-beat scanning at 320-slice CT, contrast enhancement is more homogeneous and most artifacts are eliminated. |
"This hasn't been published yet," he added, "but I think we can see better around calcium, which is one of the Achilles' heels of CT." Blooming artifacts make it harder to see around coronary artery calcium, he said. Also, when the heart is scanned in a single beat, images can be acquired with less contrast, he said.
"The contrast injected at time zero transits across the lungs into the left heart, and the concentration increases on the left side," DeFrance said. With 64-slice coronary CTA, "once the contrast peaks in the left side we have to image for eight seconds and we have to keep the contrast flowing in, [producing both] arterial and venous enhancement."
Because scan times are shorter with 320-detector-row CT, only 50-60 cc of iodinated contrast material is needed, versus the 80-100 cc needed to maintain opacification over the course of an eight-second scan with 64-slice CT. And the shorter acquisition time means that contrast opacification is more homogeneous with 320-detector-row CT.
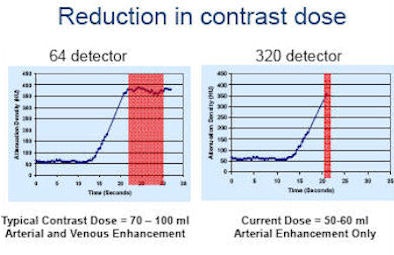 |
| By shortening the scan time to 350 msec, the duration of peak enhancement can be shortened and the contrast dose reduced from 80-100 cc to 50-60 cc for a typical coronary CTA exam. |
The lower contrast dose reduces the small risk of contrast reaction. And the shorter scan and contrast injection times not only reduce variability in opacification, they eliminate venous contamination with the contrast agent. "The image quality improvements are really because of temporal uniformity," DeFrance said.
These features also serve to get patients on and off the table more quickly, he said. "This scanner can do a wider range of patients, it can tolerate more heart rate variability, and that's what slows down the scans," he said.
|
|
|
|
| Cardiac functional analysis using one-beat scan protocol. Data are acquired over a single cardiac cycle. The mA has been lowered during the systolic phase and increased during diastole. 320-slice CT enables modulation of the mA during a single RR interval for a reduced radiation dose. Video courtesy of Dr. Tony DeFrance. |
| Having trouble viewing this clip? Click here to download the free Flash player. |
While 64-slice scanners require fairly steady heart rhythm, often 320-detector-row CT can perform scans in patients with "profound arrhythmias such as atrial fibrillation" -- using varying RR intervals for reconstruction. "In most people's labs they won't even try to do afib," DeFrance said, but with 320-detector-row CT one can at least try, though "you have to pick the cases," he said. Scanning a patient with arrhythmia and a heart rate of 110 bpm would not be feasible, "but if we have relatively controlled afib in the 60-80 [bpm] range we can do that."
The scanner also has an "arrhythmia rejection" feature that detects an abnormally short beat and shuts off the x-ray tube automatically until the next beat, DeFrance explained. If the second beat also is short, the scanner will hold off acquisition until the third beat.
Finally, with the aid of prospective electrocardiogram (ECG)-gated multisegment imaging "we can do higher heart rates, 70 or 75," he said. The scanner "will detect that and image in two separate beats -- turn on and off twice. We can move around the cardiac cycle, so even though we turn the x-ray tube on and off, we still can move to different parts of the cardiac cycle to pick out the best image."
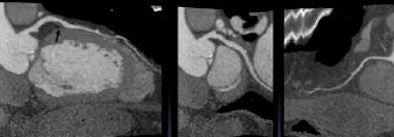 |
| Prospective ECG-gated multisegment coronary CTA is performed on a 46-year-old man with cardiomyopathy. The 320-slice CT scanner automatically chose a two-beat image acquisition to accommodate a fast heartbeat of 82 bpm. |
While providing higher spatial resolution, "using these kinds of techniques makes it applicable to a wider group of patients," he said. "We've seen a lot of flexibility with this machine because there are several protocols that can be used."
Cost and workflow implications
Although DeFrance, an interventional cardiologist by training, said that these days he performs cardiac CT mostly in outpatients, the technology has enormous potential in the hospital emergency department.
"We have 6 million people showing up a year [in U.S. emergency departments] with chest pain and very long wait times," he said. "We spend billions of dollars just for diagnostic evaluation for hospital patients. The average wait time is 13 hours. And the problem is that 85% of the people who are admitted don't have an acute coronary syndrome."
After an expensive conventional workup that includes a patient history and physical exam, cardiac enzymes, ECGs, nuclear stress testing, and more, 30%-40% of invasive coronary angiography studies are still coming back negative. And after all that "we're still missing 2%-5% of [myocardial infarctions]," he said. "It's a major cost center in the ED: lawsuits for missed chest pain."
Not only is today's chest pain workup unwieldy, but funding for the status quo is set to be reduced considerably. The Deficit Reduction Act (DRA) of 2005 already cut $1.7 billion in Medicare imaging expenditures in 2007, and indications are that the U.S. Centers for Medicare and Medicaid Services (CMS) has plans to cut billions more in imaging expenses. In this kind of environment, cardiac CT will become a critical technology, DeFrance said.
Under the CMS plan, payments will be acuity-based rather than charge-based, DeFrance said. Benchmarking standards might be used, for example, to levy stiff financial penalties on hospitals whose chest pain patients stay in the hospital longer than the national standard. Reimbursement based on the diagnosis present at admission means that additional tests may not be reimbursed, he said.
"All of that means we're going to have to change the workflow," he said "We're really going to have to find out what's going on with the patient quickly."
Cardiac CT is tailor-made for cutting costs, he said. It's fast, relatively inexpensive, and comes with a high negative predictive value, approaching 100%. In contrast, the negative predictive value for nuclear SPECT -- which, incidentally, delivers a much higher 18-20 mSv of radiation -- is about 85%, meaning that 15% of the patients undergoing myocardial perfusion imaging might end up with an undetected myocardial infarction.
Multiple studies have demonstrated that when coronary CTA is negative, the patient will not go on to have an acute coronary syndrome, DeFrance said. Studies show that the coronary CTA workup strategy has resulted in a 0%-0.6% myocardial infarction rate, no deaths at two years' follow-up, a negative predictive value of 98%-100%, and detection of noncardiac causes of thoracic chest pain in up to 25% of cases. Larger, multicenter trials in progress are expected to show more of the same.
At Johns Hopkins University in Baltimore, researchers are using 320-detector-row CT to perform adenosine perfusion stress tests, assessing myocardial viability with late contrast enhancement, in addition to the standard evaluation of the coronary arteries, valves, and chambers.
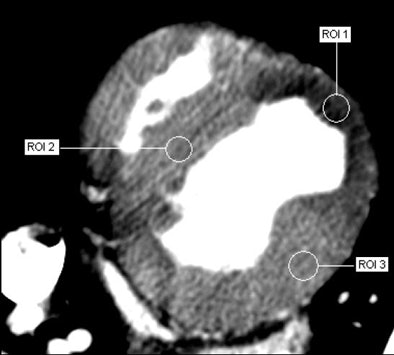 |
| Adenosine-augmented 320-slice MDCT myocardial perfusion imaging provides semiquantitative measurements of myocardial perfusion. Image courtesy of Dr. Richard George and Dr. Albert Lardo, Johns Hopkins University. |
"Hopefully that perfusion study will be under 10 mSv, and that's what people are nervous about -- that this is going to change the game," he said.
In fact, coronary CT would make an ideal gatekeeper to the cath lab, he said. In those cases when CT finds that intervention is necessary, doctors will perform it with far more information about the patient's cardiac anatomy and function than they ever had before.
Ultimately, cardiac care focused on CT will free up hospital beds and space in crowded emergency departments, DeFrance said. The result will be nothing less than a paradigm shift in patient care.
"Shift happens," he said. "I think the shift is going to change the way cardiac disease is diagnosed and treated, and my feeling is that it's going to reduce healthcare costs at a time when there's a lot of scrutiny on imaging costs, on hospital costs, etc. It looks like this technology will move us in the direction of cost savings, and I'm hopeful it will reduce morbidity and mortality and improve the patient experience."
By Eric Barnes
AuntMinnie.com staff writer
October 3, 2008
Related Reading
Coronary CTA cheaper for chest pain than standard care, September 19, 2008
Prospective gating minimizes dose in 320-slice CTA, August 5, 2008
Fourth-generation MDCT scanners do cardiac differently, July 8, 2008
Coronary CTA cuts costs for chest pain care, February 29, 2008
Radiation dose slashed in 64-slice coronary CTA, February 15, 2007
Copyright © 2008 AuntMinnie.com