Several new studies are reporting that contrast-enhanced CT can readily demonstrate myocardial infarction (MI) as foci of reduced attenuation compared with normal myocardium. The studies hint at a predictive role for CT in assessing a patient's prognosis after a cardiac event.
CT can even help establish a prognosis for the recovery of wall motion, researchers say. And since contrast-enhanced CT is already ordered routinely for a variety of indications such as suspected pulmonary embolism, routine assessment of MI could potentially wield an immediate and positive clinical impact.
As reported in the Journal of Computer Assisted Tomography, a technique developed by researchers from the University of Munich in Germany yielded moderate-to-high sensitivity for the detection of myocardial infarction, providing reliable information on both the age and size of the lesions.
A study in this month's Circulation found evidence that CT evaluation of transmural myocardial microcirculation can predict wall-motion recovery after subendocardial infarction.
Another study, in the June American Journal of Roentgenology, found that acute MI could readily be seen as foci of reduced enhancement in patients who underwent contrast-enhanced thoracic CT for other indications.
Electron-beam CT can provide insight into morphologic and functional changes after myocardial infarction, including analysis of cardiac function and myocardial infarction, wrote Dr. Konstantin Nikolaou, Dr. Andreas Knez, and colleagues from the University of Munich in Germany for the Journal of Computer Assisted Tomography.
Other CT studies have shown delayed contrast enhancement in the area of infarction up to several hours after contrast administration, and there have been case reports on the use of contrast-enhanced MDCT for this purpose without delayed imaging and the need for repeat scanning, they reported (JCAT, March-April 2004, Vol. 28:2, pp. 286-292).
"We retrospectively tried to validate the use of routine contrast-enhanced MDCT of the coronary arteries to detect myocardial infarctions," the authors wrote. "The standard MDCT angiography protocol has not been changed...no additional scan for detection of late enhancement effects was performed, and no additional radiation dose was applied to the patient."
The study looked at 106 patients (73 men, mean age 64; 33 women, mean age 59) who underwent standard contrast-enhanced MDCT coronary angiography. Complete histories were available for all cases, as well as the results of left-heart catheterization with biplane contrast ventriculography acquired within the previous eight days.
All images were acquired using a four-slice multidetector-row scanner (Somatom Sensation 4, Siemens Medical Solutions, Malvern, PA) using 4 x 1-mm collimation, 0.5-second rotation, 120 kVp and 400 mAs, in a 35-40-second scan that covered the entire heart using retrospective ECG gating. The datasets were reconstructed using 1.25-mm slice thickness and 0.7-mm reconstruction intervals. The patients received 120 ml of nonionic contrast media (300 mg iodine) with a flow rate of 3 mL/s and bolus-estimated contrast arrival time.
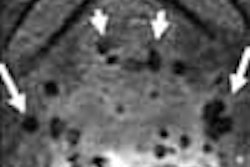
An experienced reader blinded to all results used axial images and multiplanar reformations to analyze the myocardium. Images were reconstructed in the diastolic phase (60%-70% of R-R interval) in an effort to minimize motion artifacts, and a statistical analysis was performed to evaluate sensitivity, specificity, and diagnostic accuracy for the blinded detection of infarction.
Myocardial infarctions were found in 27 of 106 patients, of which MDCT detected 23/27 correctly, for a sensitivity of 85%, specificity of 91%, and accuracy of 90%, the authors wrote.
Moreover, localization of the infarcts was precise in 15/23 (65%) of infarctions detected correctly, compared with regional wall-motion abnormality in cineventriculography, and there was "partial" agreement in six other infarctions.
Ten of the infarctions were recent and 10 were chronic, but although MDCT correctly found 7/10 to be recent infarctions, three recent infarcts were falsely seen as chronic. The infarct volumes of recent infarctions (6.3 ± 3.6 cm) showed a significant negative correlation with the ejection fraction according to contrast ventriculography. For recent infarctions, the larger the volumes as measured by MDCT, the worse the ejection fraction [r=-0.072m p=0.0190].
"Ischemic changes in the myocardium after coronary arterial occlusion consist of disruption of cell membrane function and integrity and increased permeability of small vessel wall," the group wrote. "The initial area of low attenuation primarily reflects myocardial edema (i.e., pronounced water content of the myocardium, followed by infiltration of inflammatory cells). The necrotic myocardium is subsequently replaced by fibrous or fatty tissue, which is also characterized by a reduction of attenuation in CT compared with normal myocardium. However, perfusion defects aren't specific to infarction, as severe local ischemia can produce similar perfusion inhomogeneities."
There are also variations produced by the contrast injection protocol, the authors wrote.
MDCT yielded moderate-to-high sensitivity for the detection of myocardial infarctions; however, it missed four infarctions, three of them recent. In recent infarctions, the reductions in HU are less pronounced compared to chronic infarctions.
Nevertheless, "the simultaneous depiction of the coronary arteries in considerable detail provides the opportunity to allocate the infarct area to a specific vascular supply territory," the group concluded. "Future developments in postprocessing software will enable the assessment of global and regional myocardial function from MDCT datasets."
Transmural myocardial microcirculation
In the May issue of Circulation, Dr. Hiroshi Wada and colleagues from the Omiya Medical Center and Jichi Medical School in Saitama, Japan, evaluated transmural myocardial microcirculation with contrast-enhanced four-slice MDCT to estimate the recovery of left ventricular function.
"After reperfusion therapy for acute myocardial infarction (AMI), evaluation of transmural myocardial microcirculation can indicate prognosis," they wrote (Circulation, May 2004, Vol. 68:5, pp. 512-514).
The study prospectively examined 17 patients with anterior AMI who had complete occlusion in the proximal left anterior descending artery (LAD), and who had undergone successful balloon reperfusion therapy within 24 hours of onset.
"The median of the epicardial perfusion ratio (infarcted anterior epicardial CT number/intact lateral epicardial CT number ratio = 92%) was used to categorize the cases into 2 groups: the transmural infarction group (n=8) and the subendocardial infarction group (n=9)," they wrote.
Wada and colleagues reported no significant difference between myocardial enhancement in the acute phase and anterior wall motion or ejection fraction in the acute phase. However, the transmural infarction patients had poor recovery of anterior wall motion at six months after AMI onset, while the subendocardial infarction group exhibited good recovery of regional and global left ventricular function. The authors concluded that CT can predict wall-motion recovery after acute myocardial infarction.
Acute MI detectable on single-slice
Last but not least, radiologists from the Montefiore Medical Center in New York City performed a retrospective study of 18 patients (mean age 66) with well-documented myocardial infarction who underwent contrast-enhanced CT angiography prior to their discharge from the hospital. Each case was matched by age and sex to a control group member (mean age 66) who underwent contrast-enhanced CT for any indication but had no myocardial infarction (American Journal of Roentgenology, June 2004, Vol. 182:6, pp. 1563-1566).
CT images were acquired on a single-detector scanner (HiSpeed, GE Healthcare, Waukesha, WI) with collimation of 3-5 mm, pitch 1-2, and 150 mL of nonionic contrast with a 15-30-second delay depending on the clinical indication for the scan. The images were evaluated on a workstation with a preset soft-tissue window that was occasionally adjusted by the two experienced cardiothoracic radiologists and senior radiology resident. All findings were reviewed by a senior radiology resident.
The results showed that 15/18 (83%) of patients had a focal decrease in left ventricular myocardial enhancement of 20 HU or more in the coronary artery distribution of acute MI, and the decreased enhancement was also noted visually in 9 (50%) patients (mean 50 HU, range, 8-87 HU). Six patients (33%) had a decrease of 20 HU or more (mean 74 HU, range 15-114 HU) at the site where the MI was detected quantitatively but not visually, the authors wrote. In three patients the MI was not detected on CT; one of these patients had poor blood enhancement of the left ventricular cavity. And among the controls, one healthy patient was identified as having a septal MI.
Overall, CT demonstrated sensitivity of 83%, specificity of 95%, positive predictive value of 94%, and negative predictive value of 86% for the detection of initial acute myocardial infarction.
"This series showed that initial acute MI is detectable on contrast-enhanced CT as a focal area of decreased left ventricular myocardial enhancement in a specific coronary artery distribution of the clinical infarct," the authors wrote. "This finding is clinically relevant because contrast-enhanced CT is performed for such indications as suspected pulmonary embolism and aortic dissection, which have clinical features that overlap those of acute MI. Atypical presenting symptoms occur in 20%-60% of patients with acute MI; this trend is especially true for women. If acute MI is evident on CT, the diagnosis can be suggested, leading to appropriate triage of the patient."
By Eric BarnesAuntMinnie.com staff writer
June 10, 2004
Related Reading
Stress MRI tops echo for coronary disease detection, May 26, 2004
Resting MCE may prove superior to SPECT for identifying myocardial viability, March 7, 2004
Accuracy of multidetector CT for coronary stenosis depends on patient selection, March 15, 2004
Myocardial ischemia, viability made apparent with MR, February 6, 2004
Dobutamine echo best for assessing cardiac risk with major vascular surgery, November 14, 2003
Copyright © 2004 AuntMinnie.com