
3D CT imaging of the stomach has improved to the point where it's just as useful as endoscopy for differentiating benign from malignant gastric ulcers, albeit with important differences, say researchers from Taiwan.
Their study of patients with benign and malignant gastric ulcers found that although endoscopy was more sensitive in depicting malignancy according to ulcer base, virtual gastroscopy (VG) was more specific in depicting malignancy according to ulcer margin.
Early diagnosis of stomach cancer, the second leading cause of cancer death in Asia, is crucial for improving patient outcomes, wrote study authors Dr. Chiao-Yun Chen, Dr. Yu-Ting Kuo, Ph.D., and colleagues from Kaohsiung Medical University, in Kaohsiung, Taiwan, in Radiology (published online before print, June 1, 2009).
"Patients with gastric ulcers have been found to be at greater risk for developing gastric cancer," they wrote. "Because malignancy is best treated in its early stages, it is usually recommended that all instances of gastric ulcers be followed up with conventional endoscopy and histopathologic studies until they have healed to ensure that they are not, in fact, malignant. However, because endoscopy is an expensive and invasive procedure, many patients, even those at higher risk levels, might refuse to undergo such essential endoscopic examinations."
Although CT has not been widely used for detecting stomach cancers, 3D virtual gastroscopy with air distention can now be used to provide images that are almost as detailed as those produced by using endoscopy, they wrote.
The retrospective study aimed to compare the performance of CT VG with that of conventional optical gastroendoscopy for differentiating malignant from benign gastric ulcers. Gastric ulcers in 115 patients (mean age, 64.7 years; range, 31-86 years; 61 men, 54 women) were evaluated using both endoscopy and VG.
All 76 patients with malignancies were suspected of having malignant gastric ulcers at endoscopy. The indications for 39 benign cases included seven patients suspected of having malignant gastric ulcers at endoscopy, eight patients with intractable gastric ulcers that didn't heal after eight weeks of treatment with proton-pump inhibitors, and eight patients with ulcers larger than 3 cm in diameter at endoscopy. Sixteen additional cases that were difficult to exclude at gastroscopy (n = 8) had suspicious biopsy results (n = 5) or gastric bleeding (n = 3).
Following an eight-hour fast and ingestion of gas-producing crystals to distend the stomach, 89 patients were scanned supine with MDCT using a 16-detector-row scanner (LightSpeed, GE Healthcare, Chalfont St. Giles, U.K.) with 1.25-mm collimation and a 0.625-mm reconstruction interval. An additional 26 patients were scanned on a 64-detector-row machine (Brilliance, Philips Healthcare, Andover, MA) using 0.625-mm collimation and a 1-mm reconstruction interval. All patients were scanned at 250-300 mAs and 120 kVp.
Two experienced radiologists independently created and interpreted the VG images on a 3D workstation. Malignant and benign cases were randomly intermixed, and the readers were blinded to the endoscopy results, the authors wrote.
Endoscopy was performed on each patient by one of two experienced gastroenterologists using end-viewing fiber-optic panendoscopes (GIF-XQ240, Olympus, Tokyo) after administration of oropharyngeal anesthesia. Each case was diagnosed independently, followed by a consensus evaluation.
The radiologists looked at ulcer shape, base, and margin and periulcer folds. Malignant ulcers were characterized by irregular, angulated, or geographic shape; uneven base; and irregular or asymmetric edges.
Ulcers with "disrupted or moth-eaten appearance of periulcer folds near the crater edge and/or clubbed or fused folds" were also considered suspicious, while benign ulcers were identified by their "smooth and regular shapes, even bases, clearly demarcated and regular edges, and folds that tapered and converged toward the ulcer," Chen and colleagues wrote.
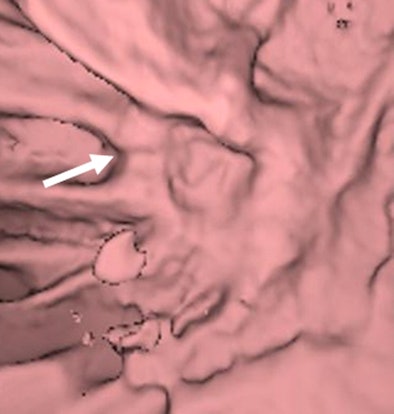 |
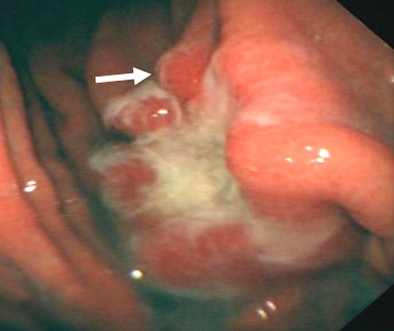
| Images of a malignant gastric ulcer in a 65-year-old man. VG image (above) shows en face view of ulcer, and endoscopic image (below) shows minimal oblique view of ulcer at the gastric part of the body with uneven ulcer base, irregular ulcer shape, irregular ulcer margin, and associated gastric folds with rugae interruption (arrows). Images republished with permission from RSNA: Chen C, Kuo Y, Lee C, et al. Differentiation between malignant and benign gastric ulcers: CT virtual gastroscopy versus optical gastroendoscopy. Radiology. Online June 1, 2009. |
 |
Histopathologic results revealed that 39 gastric ulcers were benign and 76 were malignant. VG and endoscopy yielded sensitivities of 92.1% (70/76) and 88.2% (67/76), respectively, for overall diagnosis of malignant gastric ulcers. Specificities were 91.9% (34/37) and 89.5% (34/38), respectively.
Though the techniques yielded similar results, their strengths were showcased in different types of cases. Endoscopy was more sensitive in depicting malignancy according to ulcer base, with a sensitivity of 85.5%, or 65 of 76 patients, versus VG's sensitivity of 68.4%, or 52 of 76 patients (p = 0.034). VG was more specific in depicting malignancy according to ulcer margin, with a specificity of 78.4%, or 29 of 37 patients, versus endoscopy's 63.2%, or 24 of 38 patients (p = 0.034), the authors wrote.
"VG and endoscopy had significantly different diagnostic results in the evaluation of ulcer base and ulcer margin (both p = 0.034, McNemar test)," Chen and colleagues noted.
VG's field-of-view is wider than that of endoscopy and better for evaluating high lesser curvature sites and duodenal bulbs than conventional optical endoscopy, according to the authors.
"Because views obtained with a virtual camera can be adjusted without substantial limitations, and because they can be reformed retrospectively to clear up any blind spots, VG produces better overall views of the whole ulcer and better views of the ulcer margin than endoscopy (p = 0.034)," they wrote. "Because its view comes from several angles, it offers a more precise measurement of the abnormality. Even more important, VG is technically less invasive than endoscopy."
On the downside, VG cannot depict color changes, making it difficult to detect flat lesions or evaluate subtle changes at the ulcer base, the authors noted -- two patients in the study had flat ulcers that were undetectable at VG. Endoscopy also produced better views of the ulcer base, in part due to its ability to depict color changes.
In addition, reconstruction algorithms can not produce natural-looking images, according to the authors, and endoscopy retains its better spatial resolution with a pixel size of about 0.3 mm/pixel, compared to VG's 0.59-0.82 mm/pixel.
Other drawbacks to CT is that it delivers ionizing radiation, and it does not result in biopsies that can be used for histopathologic evaluation, making optical endoscopy mandatory for confirmation of findings.
"VG and endoscopy were almost equally useful in distinguishing between malignant and benign gastric ulcers," they wrote. "The relative reduction in discomfort of the noninvasive VG examination may make it a good potential alternative means for evaluating ulcers."
Additional studies are needed to evaluate VG's overall efficacy and its cost-effectiveness, they concluded.
By Eric Barnes
AuntMinnie.com staff writer
July 21, 2009
Related Reading
Capsule endoscopy image quality not improved with oral bowel prep, July 9, 2008
Female hormones appear to influence risk for gastric cancer, December 20, 2007
X-ray screening reduces gastric cancer mortality in Costa Rica, November 19, 2007
Gastric cancer belongs to spectrum of hereditary colorectal cancer malignancies, June 28, 2007
Copyright © 2009 AuntMinnie.com



















