While computer-aided detection (CAD) technology shows promise for assisting radiologists in detecting pulmonary embolism (PE), four papers presented at the 2006 RSNA meeting in Chicago showed a wide range of sensitivity for various iterations of the technology.
Researchers from the University of British Columbia's St. Paul's Hospital in Vancouver found the CAD system they tested to be user-friendly but plagued by too many false negatives.
"High false-negative results demand technological improvement to increase the sensitivity of the system," said Dr. Zeev Maizlin, who presented the group's findings.
To evaluate the performance of a CAD system for diagnosing PE on CT pulmonary angiography studies, the researchers reviewed 104 exams, both by radiologists and ImageChecker CT v2.0 (R2 Technology, Sunnyvale, CA). CT scans were performed with 1.25-mm collimation, and were read and reported by radiologists in a routine daily clinical setting.
Later, they were retrospectively processed by the CAD system. An experienced radiologist then reviewed any discrepancies between the radiologists' reports and the CAD system findings. For the purposes of the study, emboli identified by the initial reporting radiologist and approved by the inspecting radiologist were used as the gold standard.
Radiologists identified 45 PEs in 15 patients, while the CAD system detected 26 PEs in eight patients. The CAD system also detected false-positive findings in 20 patients without PE, Maizlin said.
 |
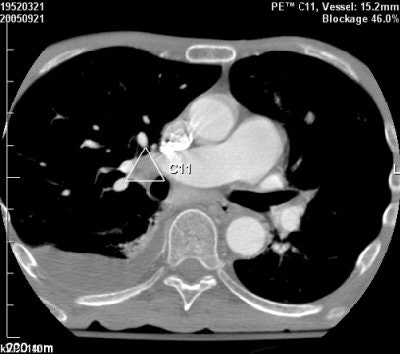
| Above, false-negative PE finding, missed by CAD system and added manually by the radiologist. Below, perivascular soft tissue that produced a false-positive PE finding from CAD. Images courtesy of Dr. Zeev Maizlin and Dr. Peter Cooperberg. |
 |
Overall, the CAD system turned in a sensitivity of 53%, specificity of 78%, positive predictive value of 29%, and negative predictive value of 90%, according to the researchers.
"Only with future advances in computer technology, CAD systems will probably become a helpful supplement to the work and eyes of the radiologist," Maizlin concluded.
Sensitivity gains
CAD showed higher sensitivity, however, in research from the University of Maryland Medical Center in Baltimore.
To evaluate CAD's performance in detecting and assessing the severity of segmental and subsegmental PE and to predict embolism severity, the researchers retrospectively selected a set of 22 positive PE cases. Two thoracic radiologists evaluated each study to establish a consensus standard of reference.
The CT studies were performed on either a 16- or 64-slice CT scanner with a slice thickness of 1.3 mm or less, according to Dr. Thomas Flukinger. He presented the research on behalf of lead author Dr. Jean Jeudy.
All cases were evaluated using an automated filling defect tool (Pulmonary Artery PE Tool, R2 Technology), and the study team determined its sensitivity for detecting PE in segmental and subsegmental arteries.
Each PE was given an obstruction index (Qanadli score) based on location and degree of obstruction. In the segmental branch, one point was given for partial obstruction and two points for complete obstruction. Proximal clots were given one point for each segmental branch, Flukinger said.
A total of 251 emboli were identified in the 22 patients by consensus evaluation; 188 were segmental and 66 were subsegmental. The CAD tool was 80% sensitive for detecting segmental emboli and 76% sensitive for detecting subsegmental emboli, Flukinger said.
There were 40 false positives, with an average of 1.8 false positives per case. As for the obstruction score, the standard of reference Q score was 35.5%, compared with 28.5% for the CAD tool.
"Overall, we found a good correspondence between CAD and radiologist-determined Q score," he said. "Further, the Q score could have prognostic value."
Flukinger acknowledged limitations of the study, including its small sample size and technical factors. False positives were common secondary to mediastinal and hilar adenopathy, as well as pulmonary veins, he said.
"Further, we needed to subtract the CAD false positives before determining the PE obstructive index," he said.
In addition, the researchers employed an early generation of CAD software, Flukinger said.
"CAD is a promising new tool in the detection of pulmonary embolism, and (it) may provide additional utility in risk stratification through the assessment of PE obstruction with a potential prognostic role," Flukinger concluded.
Image quality role
Even better results were found by researchers at Massachusetts General Hospital in Boston.
"CAD of pulmonary emboli demonstrated very high sensitivity," said Dr. Subba Digumarthy, who presented the team's research.
To evaluate the sensitivity and specificity of CAD in detecting acute pulmonary emboli in patients without significant pulmonary disease, the researchers studied 39 out of 70 consecutive patients with clinical suspicion of pulmonary embolism. Inclusion criteria for the study were good contrast opacification (HU > 250), absence of significant motion artifacts, and absence of significant pulmonary disease.
An expert panel of three thoracic radiologists reviewed the studies on an Impax PACS workstation (Agfa HealthCare, Mortsel, Belgium). The radiologists graded the studies as good or fair based on the technical factors, and assessed the studies for the presence or absence of definite emboli in the lobar, segmental, and subsegmental arteries 4 mm or larger. Discrepancies were resolved according to consensus.
The studies were then processed through ImageChecker CT v2.0 (R2 Technology), and two separate dedicated thoracic radiologists then compared the CAD results with the expert panel findings.
Of the 39 studies, 31 were graded as good and eight were judged to be fair. The studies graded as fair were attributed to artifacts due to obesity, wires, and pacemaker, and mild respiratory motion. Thirty-three patients were positive for pulmonary emboli, Digumarthy said.
Overall, CAD was 88% sensitive for all studies, and 92% sensitive in studies graded to be good. The average false-positive rate for CAD was 2.5 in good studies and 4.1 in fair studies. CAD did produce four false-negative results, including two among good studies.
Overall CAD specificity was 33% for both categories. Positive predictive value was 87% for all studies, and 85% for studies graded good.
"The accuracy of CAD improved with high-quality studies," Digumarthy concluded. "CAD in combination with radiologists detected all of the pulmonary emboli."
German research
In another paper presented at a different session at the RSNA meeting, German researchers found high sensitivity using a CAD software prototype to detect PE.
Researchers from Rheinisch-Westfälische Technische Hochschule Aachen University in Aachen sought to assess the sensitivity of the CAD software prototype (Siemens Medical Solutions, Erlangen, Germany) in detecting PE in routinely acquired multidetector-row CT (MDCT) chest examinations, particularly examining the vessel level segment.
The study included 133 patients (mean age 67 years) receiving a CT exam to rule out PE, according to Dr. Marco Das. He presented the findings at the conference.
MDCT chest exams of the thorax were acquired using a Sensation 16 16-slice CT scanner (Siemens Medical Solutions), with a standard PE protocol (120 kV, 100 mAs, 16 x 0.75-mm collimation, 1-mm slice thickness with 0.8-mm increment, and a 100-mL intravenous injection of contrast media with bolus tracking at pulmonary trunk).
All the studies were read by two radiologists to establish the reference standard, with thrombi marked at each vessel level. The CAD software was then applied to the datasets.
The software detected 79 of 92 lobar PEs, 365 of 398 segmental PEs, and 161 of 207 subsegmental PEs.
"The CAD software did not show any false-negative diagnosis in patients with PE," Das said. "The software was always positive when there was PE, even though not all PEs were detected."
The median false-positive rate per case was four, he said. With regard to vessel level, the software was 86% sensitive for lobar segments, 91% sensitive for the segmental level, and 78% sensitive for the subsegmental level.
To analyze how radiologists were performing in these cases, the researchers conducted an additional study involving a subset of 47 patients and 245 PEs.
Two radiologists -- one a first-year resident and one an experienced chest radiologist -- looked at the studies first without the software, then with the CAD software. The software increased the first-year resident's sensitivity of 74% to 85% and the chest radiologist's sensitivity of 89% to 95%, Das said.
The initial results from the CAD software are promising, Das concluded.
"The sensitivity of the software is very high, and the initial evaluation of a reader study where we use radiologists and the CAD software shows benefit for (its) use as a second reader," he said.
By Erik L. Ridley
AuntMinnie.com staff writer
January 16, 2007
Related Reading
Guidelines released for diagnostic testing in suspected pulmonary embolism, December 6, 2006
D-dimer assay can help rule out PE in low-risk patients, June 20, 2006
PET, CT CAD scheme differentiates benign from malignant lung nodules, November 28, 2006
CT lung cancer screening reduces mortality, October 26, 2006
Barriers still hinder lung CAD adoption, August 24, 2006
Copyright © 2007 AuntMinnie.com