Probably the deadliest aspect of diverticular disease is that it makes colon cancer harder to find. In the U.S., where diverticula may be present in anywhere from a third to half of the over-50 population, colon screening can be excruciatingly complex, whether performed with virtual or conventional colonoscopy. Could barium enema do a better job in some of these patients?
In a newly published study, Dr. Marc Gollub and colleagues from the Memorial Sloan-Kettering Cancer Center in New York City suggest that at least in the sigmoid colon, barium enema could potentially sidestep the chronic distension problems associated with VC in such patients, as well as the problem of incomplete colonoscopy that plagues the patients' rigid and highly tortuous colons.
In any case, the barium enema research hasn't been done yet. The present study, in which VC was performed in patients after failed colonoscopy, confirmed that elastin deposition associated with diverticular disease narrows the colonic lumen significantly, and also confounds VC evaluation (Clinical Imaging, May-June 2005, Vol. 29:3, pp. 200-206).
"Using anatomical and histological correlation, the true nature of (diverticular) disease has been well characterized and found to represent primarily a muscular disorder with resultant formation of diverticular outpouchings," Gollub and colleagues explained. "The muscular disorder is characterized by deposition of elastin in longitudinal muscle fibers (teniae coli), resulting in foreshortening of the colon. This causes a bunching up of the circular muscle fibers. No true hyperplasia or hypertrophy is found on histologic examination. This has been termed 'myochosis,' and is commonly referred to by the misnomer: 'circular muscle hypertrophy.'"
 |
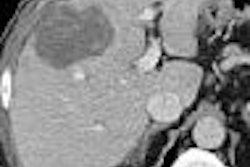
| Top left: Prone oblique CT scan of pelvis during virtual colonoscopy showing muscular thickening in sigmoid colon. Top right: multiplanar-reformatted image through muscle abnormality (myochosis) simulating a mass. Bottom left: Virtual colonoscopic view of "mass." Bottom right: double-contrast barium enema shows that "mass" is only spasm. Images courtesy of Dr. Marc Gollub. |
Pseudodiverticula form at weakness points due to herniation of the mucosa, Gollub and colleagues wrote, further describing how the muscular thickening also causes a "bunching up" of the mucosa within the lumen. Diverticular disease is most common in the sigmoid colon because it is the narrowest segment and the area of greatest intersegmental peristaltic pressure, they explained.
Although the associated colon obstruction and inflammation cause significant morbidity in and of themselves, the difficulty of finding colorectal cancer and polyps within the tortuous colonic mucosa present a difficult obstacle for detecting colorectal lesions, the team wrote.
The group examined 97 consecutive patients (mean age 62, range 30-94 years) with virtual colonoscopy (99 exams), generally as a result of incomplete optical colonoscopy (78 patients) between 1999 and 2002. The colonoscopies were incomplete due to tortuosity (n = 27), inability to tolerate procedure (n = 16), unknown reasons (n = 8), bowel fixation secondary to history of surgery leading to fixation (n = 8), diverticular disease (n = 8), poor bowel prep (n = 5), stricture or mass (n = 3), and one patient each for reaction to sedative, respiratory problems, and ventral hernia.
All but four sets of images were acquired on a four-detector-row scanner (LightSpeed QX/I, GE Healthcare, Chalfont St. Giles, U.K.) with an effective slice thickness of 3.9 mm; the first four patients were imaged on a single-slice HiSpeed GE scanner.
Prone and supine images were acquired following manual insufflation of room air, acquisition of scout images, and reinsufflation as needed. Glucagon was administered intravenously, though use of the antispasmodic agent has since been discontinued in the department due to reports that it does not improve distension, the group wrote.
Three radiologists experienced in virtual colonoscopy (range five to 80 colonoscopically proven cases) interpretation examined the images on a PACS, while blinded to the results of a previous interpretation. Colon preparation was rated poor, good, or excellent, and distension was subjectively rated on a scale of 1-4, with 4 being optimal. Evaluation of the sigmoid colon included diameter measurements in the least and most distended loop from inner wall to inner wall, and the presence of diverticula was classified as none, 1-10, or more than 10 diverticula.
"It should be noted that the sensitivity and specificity for the detection of polyps could not be determined in these patients due to the infrequent availability of colonoscopic or surgical follow-up," Gollub and colleagues cautioned. But, they wrote, the data do indicate significant limitations for visualizing the sigmoid colon due to inadequate distension compared with normal subjects. They were able to confirm the narrowed colonic lumen in patients with diverticular disease.
"In patients with muscular hypertrophy associated with diverticular disease, the minimum sigmoid colon diameter of 3.88 mm was significantly smaller than for patients without muscular hypertrophy, whether averaging prone and supine positions, or considering them separately," they wrote. "The difference was even appreciable qualitatively, where the average score was 1.56 for those with muscular hypertrophy compared with 2.18 for those without. Interestingly, the presence of simple diverticula did not alter the minimum diameter if muscular hypertrophy was absent. But indirectly, increasing numbers of diverticula were correlated with increasing likelihood of muscular hypertrophy, and this in turn was a risk for poor luminal distension."
In conventional colonoscopy, muscular rigidity and angulation of the sigmoid can prevent the colonoscope from negotiating turns and advancing into the more proximal segments.
For its part, virtual colonoscopy has significant advantages over optical or conventional colonoscopy for imaging of patients with diverticular disease, they wrote. The detection of extracolonic abnormalities, ability to examine areas not reached by the colonoscope, and direct visualization of the actual colon wall and pericolonic fat and lymph nodes also constitute advantages for VC, the authors stated.
However, direct visualization of the colon wall can be disadvantageous in the setting of myochosis, where "the appearance may be confusing, and cause difficulty in distinguishing between myochosis, tumor, or underdistension in the sigmoid colon," they wrote. And the results from several published studies show that one-third to one-half of false-positives in VC may be attributable to diverticular disease.
"Analysis of the mucosa is key, since this is where a primary epithelial tumor begins and manifests on all imaging examinations used to date," the team wrote. "For this reason, the double contrast barium enema which directly depicts the mucosa and avoids visualizing the actual bowel wall (e.g., confusing wall appearances) should provide an advantage in this scenario. Furthermore, the ability to interactively control the degree of distension during the barium examination, whether with air or additional barium, should overcome the tendency toward underdistension noted on CTC (VC) exams."
Still, the group cautioned, any advantage of double-contrast barium enema may well be limited to the affected sigmoid colon. In areas of the colon without diverticular disease and associated myochosis, virtual colonoscopy has been shown to be consistently superior.
"For this reason, we recommend alternative methods such as barium enema when patients require further evaluation of the sigmoid colon after incomplete colonoscopy in the setting of sigmoid diverticulitis," the group concluded. "If the sigmoid colon was adequately assessed, but the muscular rigidity precluded advancement of the endoscope to the more proximal colon, CTC has been well established as superior to barium enema in examination of the remainder of the colon."
By Eric Barnes
AuntMinnie.com staff writer
May 25, 2005
Related Reading
Automated CO2 insufflation improves VC, December 1, 2004
Tailor insufflation technique to the patient, says VC researcher, January 30, 2004
Virtual colonoscopy's tortuous path in diverticular disease, June 20, 2002
Copyright © 2005 AuntMinnie.com