By Sean David Wiley RPA, RT
Physicians face a difficult decision when they choose intravenous access lines for patients with serious infections. These infections can be caused by sensitive strains of pseudomonas aeruginosa, escherichia coli, proteus, klegsiella, serratia, enterobacter, acinetobacter, providencia, citrobacter, and staphylococcus (Campbell, Mauro, Jacques, 1994). The patients require long-term therapy with antibiotics such as erythromycin, gentamicin, or vancomycin, which is highly irritating and is best infused through a peripherally inserted central catheter (PICC), or a central venous catheter (CVC).
Before deciding which type of line should be inserted, physicians must evaluate a number of factors relating to the various risks, costs, and comfort levels. Are PICC lines better than CVC lines? Are they cheaper or more comfortable? How about the risk of infection? These and other questions must be reviewed and considered in depth before insertion of a PICC line or CVC line is done (Kazanjian, Daufman, 1994).
Procedure logistics
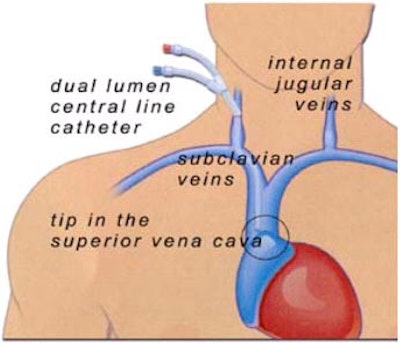
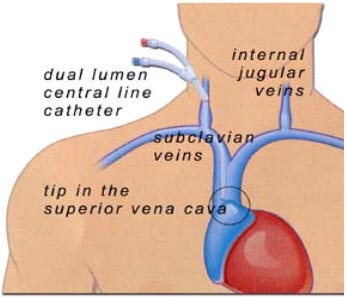
The choice of line is based on a number of variables such as patient stability, degree of infection, and duration of antibiotic therapy needed (Johnson, Oppenheim, 1992). Both procedures can be done at bedside or in the radiology department under sterile conditions with the use of a local anesthetic. PICC and CVC lines are inserted directly into the superior vena cava with line placement verified by a chest x-ray. PICC lines are generally inserted through an extremity such as the arm, whereas a CVC line is inserted through the jugular vein or subclavian (Andrews, Marx, Williams, 1992).
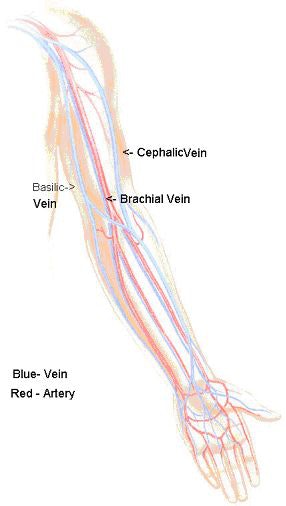 |
| Image courtesy of Sean David Wiley. |
PICCs are placed directly into the superior vena cava through the cephalic, brachial, or basilic vein of the antecubital space with the assistance of ultrasound or venography for vein selection. The vein is assessed, and a small guidewire is placed through the needle into the vein. The wire is inserted using fluoroscopy to the superior vena cava assuring vein placement. The needle is then removed over the wire and a 5-French dilator is inserted over the wire.
After the dilator is placed, the wire is marked for distance and the catheter is cut to individual length for each patient. The dilator is removed with the wire remaining in position. The catheter is then inserted over the wire and the wire is then removed after confirmation of location is achieved (Denny, 1993). PICC lines are secured in place by sutures or an adhesive dressing.
CVCs are inserted straight into the superior vena cava through the subclavian or jugular vein with the use of a fluoroscopic C-arm to insure safe placement during insertion. The patient is in the Trendelenburg position for easy access to the subclavian or jugular vein. A 19-gauge needle is introduced into the vessel and a guidewire is placed through the needle into the vein. After verification of wire placement into the superior vena cava, the needle is removed.
 |
| Image courtesy of Sean David Wiley. |
After needle removal, a dilator is placed over the wire into the vein. The dilator is then removed and the CVC line is placed. The CVC line can be placed over the wire, or a peel-away sheath can be inserted without the use of a wire (Hoshal, 1995). If the peel-away sheath is used, the sheath is placed over the wire during dilator removal, and the wire is then removed. The CVC is then placed through the sheath into the vein. One to two sutures are placed to secure the catheter to the patient, and the site is covered with a transparent dressing (Lund, Liebeman, Haire, 1999).
Risk factors
There are risks associated with placement of both PICC and CVC lines. The greatest and most common risk with both catheters is infection at insertion site (Clark, Raffin, 1998). CVC lines have a site-infection rate of 5%-55% post-insertion, while the site-infection rate for PICC lines is .05%-5% post-insertion (Bozzetti, Bonfanti, Scarpar, Ammatuna, 1993).
Other risks and complications involved with the insertion of a PICC line, but to a lesser degree, are thrombosis, hematoma, luminal thrombosis, embolism, broken catheter, and catheter extraction. Lesser risk factors for the insertion of a CVC line include pneumothorax, hemothorax, hematoma, embolism, air embolism, arterial injury, and thrombosis (Raad, Luna, Khalil, 1993).
A study with a chart review was conducted at Munroe Regional Medical Hospital in Ocala, FL, on PICC and CVC line placement in the year 2001. The researchers assessed risk factors associated with 500 patients who had undergone either PICC or CVC line insertion for long-term antibiotic therapy. All of the patients had been diagnosed with serious infection, and were receiving erythromycin, gentamicin, or vancomycin.
The group concluded that infection at the insertion site was the number-one risk for both groups of patients. Other complications that both PICC and CVC had in common were hematomas and thrombosis. Additional risks that patients might incur with these procedures are listed in table 1 and table 2.
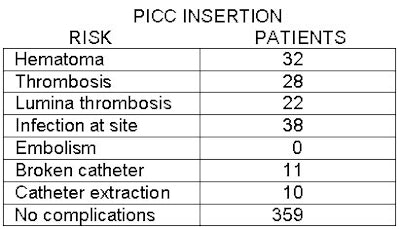 |
| Table 1 |
Table 1 lists risk factors associated with PICC insertion; table 2, risks associated with CVC insertion. Both tables provide the number of patients associated with each negative outcome. The study confirmed that both procedures come with risks and complications to the patient, but that PICC line insertion exhibited the smaller level of risk and has become the most common type of intravenous access used in patients receiving long-term antibiotic therapy.
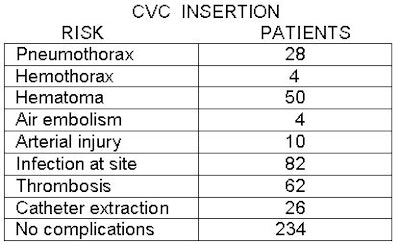 |
| Table 2 |
Cost issues
The cost for insertion of a PICC or CVC line has become a major issue in healthcare (Wickman, Purl, Welker, 1992). Due to the new healthcare reforms and reimbursement from private insurance companies, HMOs, PPOs, Medicare, and Medicaid, physicians must weigh the cost to the patient before placement of these lines can be done (Hagley, Martin, Gast, Traeger, 1992).
The cost of a PICC line tray can range from $65-$150, depending on the product and the type of material used. PICC line placements in the radiology department include the price of the line, tray, and use of the radiology room. Additional charges for placement can be for ultrasound, chest x-ray, and physician fees. Total cost for material and insertion of the PICC line can range from $600-$1,400.
The cost of placing a CVC line is almost double that of PICC line insertion, and it is extremely difficult to obtain total reimbursement from U.S. insurance companies (Orr, 1993). The cost of insertion of a CVC line is dependent on where the line is placed.
A CVC kit can cost from $100 to $350. Additional charges patients can incur include the use of a fluoroscopic C-arm, ultrasound, and a chest x-ray. The total cost of materials and insertion for a CVC line ranges from $1,600-$2,300. Due to the elevated cost for insertion of this line, more physicians are inserting PICC lines than CVC lines in the radiology department (Kazanjian, Kaufman, 1994).
Post-procedure protocol
Of course, patients receiving long-term antibiotic therapy want to minimize discomfort while maintaining their independence. Patients who are able to be discharged and receive their antibiotic therapy at home with the aid of a home-health nurse, or as an outpatient, prefer PICC lines over CVC due to the anatomical placement of the catheter (Andrews, Marx, Williams, 1992).
PICC lines are generally placed in the upper arm, which can be covered by the sleeve of a shirt, and patients can continue their normal daily activities without concern of dislodging or pulling out the catheter (Andrews, Marx, Williams, 1992). CVC lines are placed in the neck or chest areas, which can be difficult to disguise with clothing, and generally patients do not resume their daily activities because of exposure of the catheter and fear of extraction (Hoshal, 1995).
Of all the patients who are discharged from the hospital with a CVC line, 65% are admitted to a rehabilitation facility until therapy is completed (after 6-12 weeks) because of hospital protocols and policies surrounding the risks and demanding care of the CVC line (Hoshal, 1995). These patients give up a part of their independence while in rehabilitation, seem to take longer to recover, and even exhibit signs of depression (Denny, 1993).
A survey was sent to 200 patients who were discharged from Munroe Regional Medical Center in Ocala, FL, with either a PICC or CVC line inquiring as to complaints and satisfaction on the comfort of the line while they were receiving antibiotics as outpatients. The survey was designed with boxes to check "satisfied" or "dissatisfied." Questions on the survey involved line placement, patients' ability to resume a daily routine, fear of pulling out the line, and comfort.
Of the 200 surveys distributed, 148 patients responded, including 78 respondents with CVC lines and 70 with PICC lines. Among the PICC patients, most were satisfied. The two favorite features of PICC lines, from the patients’ point of view, were line placement in the upper arm and the ability to resume a daily routine. Patients who were discharged from the hospital with a CVC line had minimal satisfied marks; the two top complaints were line placement in the neck and fear of pulling out the line.
With advancements in medical technology, patients are able to be discharged from hospitals earlier and receive more of their treatment as outpatients. The use of ultrasound and venography for insertion of a PICC line has made it possible for physicians to perform interventional procedures with minimal risk to patients. Although the insertion of a CVC line does exhibit greater risk to the patient than insertion of a PICC line, the use of fluoroscopy has decreased the risks to patients by approximately 45% (Hoshal, 1995).
In conclusion, in a comparison of PICC to CVC lines through literature review, chart review, and patient surveys, a PICC line insertion is favored two to one by patients and physicians due to the lesser risk of secondary injury to patients, cost efficiency to both patients and insurance companies, and improved patient satisfaction.
By Sean David Wiley, RPA, RTAuntMinnie.com contributing writer
February 24, 2003
Sean David Wiley is a recent graduate of the radiology practitioner assistant program at Weber State University in Ogden, UT. Prior to that, he was an interventional radiology technologist for 10 years. He will soon be an RPA at the department of interventional radiology at Shands Healthcare, University of Florida, in Gainesville.
References
Andrews, J.C., Marx, M.V., & Williams, D.M., The upper arm approach for placement of peripherally inserted central catheters for protracted venous access, American Journal of Roentgenology, 1992, Vol.158, pp.427-429.
Bozzetti, F., Terno, G., Bonfanti, G., Scarpar, D., Scotti, A., & Ammatuna, M, Prevention and treatment of central venous catheter sepsis, Annual Surgeons Journal, 1993, Vol. 98:28, pp. 52-60.
Campbell, W.E., Mauro, M.A., Jacques, P.F., Radiological insertion of long-term venous access devices, Seminar in Interventional Radiology, 1994, Vol.11:44, pp.366-376.
Clark, D.E., Raffin, T.A., Infectious complications of long-term central catheters, Critical Care Medical Journal, 1998, Vol. 97, pp. 966-972.
Denny, D.F., Placement and management of long-term central venous access catheters and ports. American Journal of Roentgenology, 1993, Vol. 161, pp. 385-393.
Hagley, M.T., Martin, B., Gast, P., Traeger, S.M., Infectious and mechanical complications of central venous catheters placed by percutaneous venipuncture, Critical Care Medical Journal, 1992, Vol. 20, pp.1426-1430.
Hoshal, V., Total intravenous nutrition with peripherally inserted central venous catheters. Archives of Surgery, 1995, Vol. 43, pp. 1937-1943.
Johnson, A., Oppenheim, B.A., Vascular catheter related sepsis: diagnosis and prevention. Journal of Hospital Infection, 1992, Vol. 20, pp. 67-78.
Kazanjian, S., Kaufman, J., Strategies for central venous catheter placement in patients with limited access, Seminars in Interventional Radiology, 1994, Vol. 4, pp. 377-387.
Lund, G., Liebeman, R.P., Haire, W.D., Central Venous Catheters. Seminars in Interventional Radiology, 1999, Vol. 6:3, pp. 162-175.
Orr, M.E. (1993). Issues in the management of percutaneous central venous catheters. Nursing clinics of North America, 28 (4), 911-919.
Raad, I., Luna, M., Khalil, S.M. (1994). Relationships between the thrombotic and infectious complication of central catheters. Journal of the American Medical Association, 271, 1014-1016.
Wickman, R., Purl, S., Welker, D. (1992). Long-term Central Venous Catheters. Seminars for Oncology Nursing, 8, 133-147.
Copyright © 2003 Sean David Wiley