The Affordable Care Act (ACA) may be behind recent increases in colorectal and breast cancer screening among the lower socioeconomic groups that benefit from being insured by it and Medicare, a new study in Cancer reveals.
One goal of ACA was to reduce financial barriers for preventive healthcare services, which it accomplished via a cost-sharing provision, according to researchers from the American Cancer Society and Emory University. In the current study, Stacey Fedewa and colleagues investigated whether that provision had the effect of increasing population screening rates (Cancer, June 4, 2015).
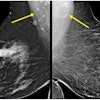
Using data from the National Health Interview Survey (NHIS), the group compared colorectal and breast cancer screening prevalence among individuals covered by private insurance and Medicare before and after ACA was implemented. They analyzed responses from 15,786 adults between the ages of 50 and 75 in the colorectal cancer screening analysis, along with responses from 14,530 women ages 40 and older in the breast cancer screening analysis.
Colorectal cancer screening rose from 57.3% to 61.2% between 2008 and 2013. The increase was seen in low-income, least-educated, and Medicare-insured individuals presumed to benefit most from the ACA, but not among higher socioeconomic groups. Five years earlier, an increase in colorectal cancer screening was also measured, but rates rose across all socioeconomic groups, the authors noted.
The encouraging results may reflect ACA's removal of financial barriers to screening, but they may also reflect a continuation of a rising trend toward screening in the affected groups, they wrote.