In their prospective multicenter study, Young Jun Kim, MD, and colleagues examined the feasibility rate for ultrasound-guided percutaneous RFA based on ultrasound for procedure planning in patients with small (≤ 3 cm), single HCCs who were initially considered to be treated with percutaneous RFA. For patients in whom the procedures weren't feasible, the researchers examined the reasons.
The study included 401 patients, and the group had a mean tumor size of 1.8 cm. Based on ultrasound planning, ultrasound-guided RFA was feasible in 248 (62%) and not feasible in 153 (38%) of the cohort.
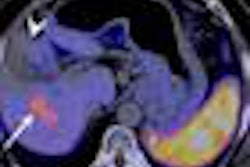
The reasons for unfeasibility included lesion inconspicuity (n = 101, 66%), unsafe electrode path (n = 17, 11%), high risk of heat sink effect (n = 13, 9%), collateral thermal damage of adjacent organs (n = 11, 7%), and high risk of central bile duct injury (n = 8, 5%). A large number of patients with small HCC lesions are not amenable to percutaneous RFA, despite being technically suitable for it, Kim will report.
"For HCC cases in which ultrasound-guided RFA is not feasible, we can do transcatheter arterial chemoembolization, surgical resection, or RFA with special [techniques] such as contrast-enhanced ultrasound, artificial ascites, and artificial pleural effusion," Kim told AuntMinnie.com.