Adult Respiratory Distress Syndrome (ARDS):
View cases of ARDS
Clinical:
Patients with ARDS present with the acute onset of dyspnea, diffuse pulmonary opacities, severe hypoxemia with a partial pressure arterial oxygen tension to fraction of inspired oxygen ratio less than 200 mm Hg, rapid respiratory failure and no evidence of congestive heart failure are said to have the adult respiratory distress syndrome (ARDS) [4,7]. Although no single pathologic sequence has been identified, it is strongly suspected that inappropriate activation of the complement cascade with release of C5a fragments directly results in increased capillary permeability. The C5a fragments also attract circulating PMN's and macrophages to the lungs where they release toxic radicals that produce inflammation and acute alveolar epithelial damage. ARDS is divided into pulmonary and non-pulmonary causes [7]. Etiologies of ARDS include: trauma, sepsis, intravascular coagulopathy, drug reaction, aspiration, pneumonia or smoke/toxic inhalation [5]. Affected patients typically have normal pulmonary capillary wedge pressures, unless their condition is complicated by superimposed left ventricular failure. Pneumothorax is a frequent complication (25-80%) and is most likely related to the use of positive pressure mechanical ventilation in these patients. The mortality rate in patients with ARDS can be as high as 60%. Increased mortality is seen in association with ventilator-associated pneumonia [4], age over 70 years [9], and underlying liver cirrhosis [9].
The pathologic findings of ARDS are divided into three stages: 1) exudation (edema, hemorrhage, and hyaline membranes); 2) proliferation (organization); and 3) fibrosis.
X-ray:
During the initial 12 to 24 hours, radiographs may fail to demonstrate an abnormality. As ARDS progresses, one sees the more classic findings of patchy (earlier) or diffuse air space disease, combined with a normal heart size, and normal vascular pedicle. Interstitial abnormalities (septal lines) are typically absent, although their presence has been reported in 0 to 40% of patients [5]. Pleural effusions are uncommon on radiographs [5]. As the exudative phase gives way to the proliferative and fibrotic phases, the radiographic appearance changes from relatively homogeneous consolidation to a mixture of ground-glass opacity, parenchymal distortion (due to the fibrosis), and cyst formation [5]. If patients survive, radiographic abnormalities typically slowly resolve over several weeks, although about 10% of patients will have residual pulmonary opacities. Differentiation of ARDS from hydrostatic edema can be difficult, but features which favor ARDS include: 1) a peripheral rather than perihilar distribution of abnormalities (unfortunately, this pattern is identifiable in less than 50% of cases); 2) absence of visible interstitial abnormalities; and 3) findings are slow to clear (hydrostatic edema typically clears quickly after the patients hemodynamics have improved) [5].
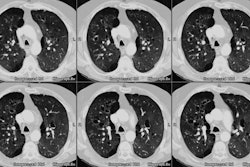
CT findings in ARDS are variable. Very early findings include patchy areas of ground-glass or air-space consolidation. Thickening of the interlobular septa (Kerly lines) is not a prominent feature, but modest interstitial abnormalities may be evident [5]. When alveolar filling begins to occur, the radiographic findings are indistinguishable from hydrostatic pulmonary edema. The typical distribution of findings on CT is bilateral dependent dense opacities that bend to regions of ground-glass attenuation, and then aerated lung in the non-dependent regions [8]. This appearance is felt to be related to edema and hyline membrane formation with collapse of the dependent regions (PEEP can reopen previously collapsed pulmonary units and reduce the amount of non-aerated lung) [4]. Areas of parenchymal consolidation can also be be seen in ARDS and cannot be used to distinguish patients with infection from those without pneumonia [4]. However, areas of asymmetric consolidation or a heterogeneous appearance are often suggestive of a pulmonary cause for ARDS and likely indicate the site of initial lung injury [7,8]. Pleural effusions are uncommon in ARDS unless complicated by superimposed infection, although other authors claim effusions can be identified in roughly half of cases [7]. ARDS is frequently complicated by widespread pulmonary vascular thrombosis and its presence is associated with an over 90% rate of mortality.
On follow-up CT, there is frequently a coarse reticular pattern with ground glass opacities in an anterior distribution. The findings are felt to be related to fibrosis secondary to alveolar overdistention (ventilator) and oxygen related lung injury. The basilar portions of the lungs are relatively spared as these regions are typically densely consolidated during the acute episode of ARDS [6].
REFERENCES:
(1) Radiol Clin North Am 1991; Sep 29 (5):943-963
(2) Radiol Clin North Am 1996; Jan 34(1):33-46
(3) Radiol Clin North Am 1996; Jan 34(1): 59-81
(4) Radiology 1998; Winer-Muram HT, et al. Ventilator-associated pneumonia in patients with adult respiratory distress syndrome. 208: 193-199
(5) J Thorac Imag 1998; Ketai LH, Godwin JD. A new view of pulmonary edema and acute respiratory distress syndrome. 13: 147-171
(6) Radiology 1999; Desai SR, et al. Acute respiratory distress syndrome: CT abnormalitis at long-term follow-up. 210: 29-35
(7) Radiology 1999; Goodman LR, et al. Adult respiratory distress syndrome due to pulmonary and extrapulmonary causes: CT, clinical, and functional correlations. 213: 545-552
(8) Radiology 2001; Desai SR, et al. Acute respiratory distress syndrome caused by pulmonary and extrapulmonary injury: A comparative study. 218: 689-693
(9) Radiololgy 2006; Ichikado K, et al. Prediction of prognosis for acute respiratory distress syndrome with thin-section CT: validation in 44 cases. 238: 321-329