Pertechnetate Imaging
Meckel's Diverticulum
Clinical:
A Meckel's diverticulum represents a persistence of the
omphalomesenteric (vitelline)
duct at its junction with the ileum (the diverticulum therefore
arises from the
anti-mesenteric border). Meckel's are found in about 2% of the
population and the great
majority of patients are asymptomatic (80%). Ectopic mucosa is
found in about
60% of Meckels and it is most commonly gastric (about 90% of
cases) [1]. If symptomatic, patients usually present by
age 2 years (60% of cases) and symptomatic lesions are more common
in males (3:1).
Symptoms in children include painless blood per rectum (most
common
manifestation), while adults most often present
with Meckel's diverticulitis. Meckel's are typically located
approximately 2 feet from the
ileocecal valve.The rule of "2's"- 2 feet from the ileocecal
valve, 2 inches in length, 2% of the population, 2 times more
common in males, and often presents in the first 2 years of life
[3].
Complications are seen in 20% of patients and include:
- Bleeding (most common complication): Generally more common in those lesions lined by gastric mucosa (found in 95% of bleeding lesions). Ectopic gastric mucosa is found in 15-25% of Meckel's, but in about 50% of symptomatic patients [2].
- Intussusception, Bowel obstruction, Volvulus
- Diverticulitis
Radiographic and Nuclear Medicine Exam Findings:
Radiographic findings on the barium exam include a wide mouth diverticulum which contains a normal small bowel fold pattern.
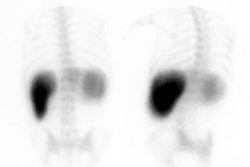
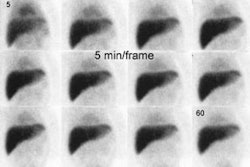
Tc99m-pertechnetate is the agent used for scintigraphic imaging as pertechnetate will accumulate within the mucous producing cells of the gastric mucosa. A dose of 10 mCi (370 Mbq) IV (50-200 uCi/kg in children) is used [3]. An area of at least 2 cm2 of mucosa is necessary for successful scintigraphic visualization. Sensitivity for the exam is over 80-90% in children, about 60% in adults (symptoms in the adult age group are usually unrelated to the presence of ectopic gastric mucosa). *Perchlorate should NOT be given prior to the exam as it will decrease gastric uptake of the tracer. Gastric concentration usually begins 5 to 10 minutes post injection, and then increases in intensity over time. Ectopic gastric mucosa demonstrates a similar pattern of tracer accumulation.
A positive scan demonstrates a focal area of increased activity in the RLQ which appears at the same time as the stomach and increases in intensity in a similar manner. On the lateral view, the activity should be unrelated to ureteral activity.
Visualization of a Meckel's diverticulum may be improved by certain pharmacologic interventions [1]:
Cimetidine: A histamine-2 receptor antagonist which will
inhibit secretion of pertechnetate by gastric mucus cells
without impairing uptake [1]. Adult patients should be
pretreated with 300 mg of cimetidine p.o. Q.I.D. for 24 to 48
hours prior to the exam [1]. A single intravenous dose of 300 mg
in 100 mL of 5% dextrose in water given over 20 minutes followed
by imaging in one hour may be used as an alternative [1]. In
children, a cimetidine dose of 20 mg/kg per day is recommended
[1]. Ranitidine can also be used at a dose of 1 mg/kg (maximum
dose 50 mg) infused over 20 minutes with imaging beginning one
hour following the infusion [1].
Pentagastrin (Pentavlon): Pentagastrin stimulates uptake
of pertechnetate in gastric mucosa (increases uptake by
approximately 30%), but also stimulates peristalsis and
secretion. Dose is 6 micrograms/kg given subcutaneously [1]. The
agent should not be given with cimetidine because the latter
antagonizes pentagastrin's stimulation of pertechnetate uptake
[1].
Glucagon: Glucagon relaxes smooth muscle and decreases
peristalsis of the stomach, duodenum, distal small intestine,
and colon [1]. The agent therefore decreases the rate at which
activity leaves the stomach and enters the small bowel.
Following the I.V. administration of 0.5 mg of glucagon peak
activity occurs between 2 to 4 minutes and last for 10 to 17
minutes [1]. Unfortunately, glucagon decreases pertechnetate
uptake in the stomach by as much as 39% and it should be used in
conjunction with pentagastrin. Nasogastric suction has also been
used to enhance imaging by removing secreted Tc-pertechnetate
activity from the stomach, thereby reducing background activity.
- Any cause of focal hyperemia: Hemangioma (usually multiple), AVM, Vascular tumor [2]
- Duplication cyst containing gastric mucosa
- Intussusception [2]
- Inflammation/Appendicitis/Abscess [2]
- Crohn's Disease
- Renal pelvis or collecting system activity [2]
- Uterine Blush: Menstruating females [2]
Retained Gastric Antrum:
The retained gastric antrum syndrome occurs in patients who have undergone partial gastrectomy with a Billroth II anastomosis. The gastrin secreting cells of the antrum are no longer inhibited by gastric acidity and the resultant increased acid output by the stomach leads to recurrent marginal ulceration. Pertechnetate imaging can be used to identify the presence of gastric mucosa in a retained antrum. The sensitivity of the exam has been reported to be about 75% with a specificity of nearly 100%.
Normally, there should be no activity identified in the region of the pylorus/duodenum in these patients. Retrograde filling of the afferent loop can be seen on cinematic display of acquisition images.
Barrett's Esophagus
Accumulation of Tc-pertechnetate in the lower esophagus after I.V. administration is considered a positive examination for the mucous secreting cells of Barrett's mucosa. Unfortunately, swallowing of free Tc-pertechnetate in the saliva and reflux of gastric activity can cause significant problems with scan interpretation. Currently, scintigraphy plays no definitive role in the evaluation of patients with suspected Barrett's esophagus.
Salivary Gland Imaging
The agent used for salivary imaging is Tc-pertechnetate. Images are obtained before and following lemon sucking. Quantitative assessment of salivary function is performed. A normal pre-lemon thyroid to salivary ratio is about 1:1 or 2:1. Decreased salivary activity can be seen in such conditions as Sj?grens syndrome.
This procedure can also be used to evaluate the parotid glands for detection of Warthin's tumor (papillary cystadenoma lymphomatosum), a benign neoplasm of the major salivary glands (particularly the parotid gland). Warthin's tumor is the second most common benign parotid tumor (after mixed tumors) and it is the most common salivary tumor to be bilateral (3-8%) or multifocal (4-12%). The lesion usually presents as an asymptomatic, painless swelling at the lower pole of the parotid gland in the sixth or seventh decade. The lesion is slow growing and may appear static over many years. Surgery is considered curative in the management of Warthin's tumor, but there is a post-op recurrence rate of about 10%.
The exam of the parotid consists of 60 second images obtained for 20 minutes after the I.V. administration of 5 mCi of Tc-pertechnetate. Waters, right, and left lateral images are then obtained. Washout images are obtained 3 minutes after stimulation with orally administered lemon juice. Warthin's tumors will typically demonstrate a homogeneously increased concentration of pertechnetate (50%) with poor clearance of tracer from the tumor following salivary stimulation. A washout pattern that shows unchanged or even increased activity is quite unique for Warthin's tumor. Poor secretion of the tracer occurs because the tumor does not communicate with the glands ductal system. A non-homogeneous or mixed pattern of activity can also be seen and is associated with cystic inclusions within the tumor. Oxyphilic adenomas (Oncocytoma) may also show increased tracer concentration. Some pleomorphic adenomas can demonstrate mild increased uptake of the tracer.
False-positive scans may also occur secondary to partial obstruction of the parotid duct, stasis or pooling of secretions within dilated acini and ducts (as in Sj?gren's syndrome), a contralateral hypofunctioning gland. Increased tracer accumulation within the parotid may also be seen in acute parotitis, but the washout pattern should be normal in this condition.
REFERENCES:
(1) Radiographics 2002; Saremi F, et al. Pharmacologic interventions in nuclear radiology: indications, imaging protocols, and clinical results. 22: 477-490
(2) Radiology 2005; Case 86: Meckel diverticulum with massive bleeding. 236: 836-840
(3) J Nucl Med 2016; Grady E. Gastrointestinal bleeding scintigraphy in the early 21st century. 57: 252-259