Radiologists can predict the presence of invasive cancer with fairly high accuracy, but their accuracy dips when it comes to predicting ductal carcinoma in situ (DCIS), according to a study published in the April issue of the American Journal of Roentgenology.
The findings speak to the need to distinguish DCIS from invasive cancer to better handle its management, especially because treatment options for DCIS are evolving -- perhaps even to hormone therapy rather than surgery, wrote a team led by Dr. Shadi Aminololama-Shakeri of the University of California, Davis.
"Current BI-RADS assessment categories estimate the overall likelihood for malignancy without attempting to distinguish between the likelihood of ductal carcinoma in situ and that of invasive cancer," the authors wrote. For women being treated for DCIS nonsurgically, "it would be important to accurately exclude the possibility of invasive disease."
Measuring accuracy
There hasn't been much research on the feasibility of separately evaluating the likelihood of DCIS and invasive cancer based on radiologists' interpretation of imaging features, according to Aminololama-Shakeri and colleagues. So the group sought to assess whether predictions by radiologists of the likelihood for DCIS and invasive cancer would correlate with known histologic outcomes (AJR, April 2017, Vol. 208:4, pp. 933-939).
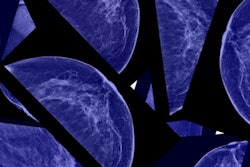
To do this, the researchers culled 250 cases categorized as BI-RADS 4 or 5 from four University of California medical centers. Ten academic breast imaging radiologists reviewed the cases, assigning each a BI-RADS category, estimating the percent likelihood of DCIS or invasive cancer, and designating a confidence rating based on a scale of 1 to 5 (1 = low, 5 = high) after reviewing screening and diagnostic mammograms as well as ultrasound images. The researchers then generated receiver operating characteristic (ROC) curves based on likelihood estimates for the presence of invasive cancer and DCIS assigned by each reader.
Of the 250 test cases, 62% were benign and 38% were malignant. There were 26 cases of DCIS (10%), 20 invasive cancers (8%), and 48 cases of invasive cancer with DCIS (19%).
The group found that the area under the curve (AUC) values for the 10 radiologists ranged from 0.83 to 0.91 for predicting the presence of invasive cancer (an AUC of 1 indicates perfect accuracy). AUC values for predicting the presence of DCIS were lower, ranging from 0.73 to 0.83, while values for predicting DCIS as a concomitant finding with invasive cancer were lower still, ranging from 0.58 to 0.78.
Aminololama-Shakeri and colleagues did not find a correlation between radiologists' years of experience and the estimated AUC for invasive cancer and DCIS.
Mind the gap
Why was radiologists' accuracy lower when it came to estimating the presence of DCIS with invasive cancer? It may have to do with disease characteristics, the authors wrote: Features of invasive cancer can be more dramatic than those of DCIS -- which tends to manifest as microcalcifications -- perhaps leading to bias toward an invasive cancer estimate.
"The presence of findings characteristic of invasive cancer supersede concomitant presence of microcalcifications or findings of DCIS in the same lesion, thereby possibly biasing the likelihood estimate toward the invasive component and minimizing the DCIS likelihood estimate," the group wrote.
The study did have limitations, according to the authors, including a lack of prior exams and a small number of DCIS-only cases. In any case, the findings suggest more research is needed on radiologist accuracy when it comes to predicting DCIS.
"Training, including review of microcalcification characteristics, before future reader studies may be undertaken to evaluate its utility in increasing [accuracy]," they concluded.