Radiation therapy with yttrium-90 (Y-90) microbeads is making strides, as witnessed by presentations at last month's Society of Interventional Radiology (SIR) meeting. Papers at the San Francisco meeting covered topics ranging from personalized dosimetry to just how close loved ones can get to patients who have received Y-90 therapy.
One size no longer fits all for administering the optimal dose of yttrium-90 microbeads for hepatic radioembolization therapies, according to a Singapore interventional radiologist, who demonstrated that controlled doses can be selectively directed to four regions of the liver for maximum therapeutic effect.
The study by Dr. Farah Irani from Singapore General Hospital was one of 13 inquiries that examined the safety and efficacy of hepatic Y-90 radioembolization. The large number of abstracts devoted to Y-90 selective internal radiation therapy (SIRT) at the SIR meeting reflects the growing role interventional radiologists play in performing radioimmunotherapy procedures first introduced at nuclear medicine meetings more than decade ago.
"Radioimmunotherapy requires support and logistics from several medical specialties," Dr. Charles Nutting, chief of interventional radiology at Sky Ridge Medical Center in Lone Tree, CO, told AuntMinnie.com. "However, the lion's share of therapy is falling to interventional radiologists."
Gaining acceptance
Y-90 SIRT is gaining acceptance, particularly for inoperable metastatic liver cancer treatment. SIRT involves catheter-based infusions of glass or fiber microspheres containing yttrium-90. The therapy is introduced into the hepatic arteries, which feed blood to the liver. Because many liver tumors are hypervascular, the particles are trapped in angiogenic microvasculature surrounding them. Beta particle emissions kill nearby cancer cells but spare more distant normal tissue.
In her SIR talk, Irani presented findings from a small, prospective trial that showed the clinical effectiveness of her group's alternative to conventional methods using patient liver mass or body surface area to calculate Y-90 dosage. When analyzed strictly as brachytherapy, Y-90 SIRT based on her approach resulted in tumor regression in all eight patients with inoperable hepatocellular carcinoma (HCC). Mean tumor size decreased 58%, though one patient progressed after three months. No significant toxicities were reported.
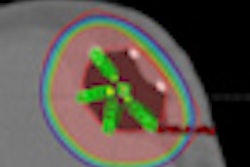
The partitioning method used to calculate Y-90 for these patients is more labor-intensive than the two standard approaches, but it is more scientifically sound, Irani said. It involves the delineation of partitions for the lung and tumor and nontumorous liver to optimize dose to specific regions of the liver.
Artery-specific perfused liver volume calculations are based on CT hepatic angiography and conventional digital subtraction angiography. Data from planar technetium-99m (Tc-99m) macroaggregated albumin (MAA) measure liver-to-lung shunt, and SPECT/CT images are used to calculate the ratio of tumor to normal liver.
Custom dosing strategies in the trial were applied for each patient. Irani showed an example of a patient with a recurrent HCC tumor at the resection margin in segment 4. The malignancy was supplied by both left and right hepatic arteries. An elevated tumor-to-normal-tissue ratio from the left hepatic artery led the interventional team to increase the dose introduced into that artery. A lower dose was administered to the right hepatic artery to protect normal tissue in the right liver lobe.
Encouraging long-term survival
In another SIR talk, Dr. Khairuddin Memon described encouraging long-term results for 80 patients treated at Northwestern University with Y-90 radioembolization for hepatic colorectal metastases.
Overall survival from Y-90 SIRT was 10.6 months. It was 32.3 months from the diagnosis of hepatic metastases, and 30.5 months from the diagnosis of the primary colorectal tumors.
Survival after Y-90 therapy was significantly longer among patients who received two or fewer cytotoxic drugs before radioembolization than among patients who received three or more cytotoxic treatments (p < 0.0001). Survival was also significantly longer after Y-90 therapy for patients who were not treated with a biologic agent, such as Avastin, compared with patients who were treated with such drugs (p < 0.0001).
Memon concluded that Y-90 treatment should be considered for second-line therapy after first-line chemotherapeutic options fail.
Y-90 SIRT for colon cancer metastases
The results were similar, though more preliminary, from a phase I trial involving 19 patients at Memorial Sloan-Kettering Cancer Center, which demonstrated that Y-90 SIRT can be safely performed on patients who fail hepatic pump and systemic chemotherapy for colon cancer liver metastases.
No dose-limiting toxicities were observed among three patient cohorts that received 70%, 85%, and 100% of the calculated dose of Y-90 microspheres.
Therapeutic responses were encouraging. Metastatic liver disease for 12 patients (70.6%) either stabilized or responded positively. Five patients (29.4%) progressed, and postprocedural results were still pending for two patients.
Y-90 safety goes beyond NRC regs
Regulation of Y-90 SIRT was the focus of a SIR presentation by Dr. Jeffrey McCann of Thomas Jefferson University. He found that providers should have no trouble meeting the U.S. Nuclear Regulatory Commission (NRC) regulation governing the safe discharge of patients after Y-90 administration. However, his results suggest a need to focus on possibly high exposures to caregivers, children, and pregnant women.
The NRC allows patients to be discharged without receiving safety instructions if the total effective dose (TED) to nontreated people exposed to the patient is less than 1 mSv (43 µSv/hour).
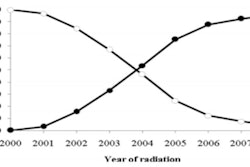
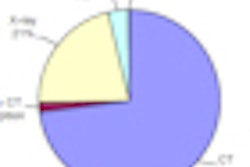
The threshold for action called for by the federal regulation, however, is more than three times the maximum exposure rate McCann and colleagues measured from 804 Y-90 SIRT patients at six hospitals. He reported that 514 of those subjects were treated with SIR-Spheres (Sirtex Medical) and 290 received TheraSpheres (Nordion), the two agents approved by the U.S. Food and Drug Administration (FDA) for hepatic radioimmunotherapy.
The average dose rate for SIR-Spheres was 1.8 µGy/hour, with a maximum rate of 16 µGy/hour. The average for TheraSpheres was 1.9 µGy/hour, with a maximum of 12 µGy/hour.
The NRC regulation is based on an occupancy factor of 0.25, the equivalent of standing 1 meter from the patient for six hours, McCann noted. An alternative standard, offered by Dr. Seza Gulec, chief of surgical oncology at Jackson Memorial Hospital in Miami, proposes an occupancy factor for a sleeping partner of 0.25 at a distance of 0.3 meter, producing a TED 10 times higher than the NRC requirement. Gulec's occupancy rate of 0.042 at a distance of 0.1 meter produced a TED five times higher for infants, children, and pregnant women.
Based on Gulec's standards, 23% of patients administered SIR-Spheres and 21% who received TheraSpheres exceeded the 1-mSv threshold for frequent caregivers.
For a sleeping partner, 7.8% of patients administered SIR-Spheres and 10% who received TheraSpheres exceeded the threshold. For infants, children, and pregnant women, 2% who received SIR-Spheres and 3% who were given TheraSpheres exceeded 1 mSv.
Patients who exceeded the 1-mSv threshold for the restrictive scenario had a high administered activity or a low body mass index, McCann said. TED may be influenced by tumor position and measurement geometry.