Top Story
Latest News
State of the RT profession more palpable than ever
April 24, 2024
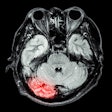
Cases of the Week
Check out our Cases of the Week!
More from AuntMinnie
Esaote reports growth in fiscal year 2023
April 25, 2024
Next Generation Radiology Workflow Tools
April 24, 2024
Voiant and Thirona enter commercial partnership
April 24, 2024
Spectral AI names CEO of Spectral IP, plans spin-off
April 24, 2024