Researchers at the University of Pennsylvania are advancing lung cancer surgery by combining intraoperative molecular imaging (IMI) with a novel near-infrared contrast agent and preoperative PET/CT scans to help surgeons better see and extract both obvious and hard-to-find tumors.
 Dr. Jarrod Predina.
Dr. Jarrod Predina.Preliminary results from a pilot trial, published online July 25 in the Annals of Surgery, show how the infrared agent, OTL38, makes tumor cells glow, allowing clinicians to detect malignant lung nodules as small as 0.5 mm. When used with intraoperative molecular imaging, OTL38 guidance was also credited with finding more lesions that went unseen in preoperative PET/CT scans.
"In about 1 out of 10 patients, we found cancer that was otherwise completely undetected," said lead author Dr. Jarrod Predina, a postdoctoral research fellow in Penn's Thoracic Surgery Research Laboratory. "It changed our management plans; it changed the staging of the patient; and that additional information changed the patient's postoperative course in terms of chemotherapy and radiation."
Effective extraction
OTL38 is an investigational agent that combines fluorescent dye and a folate facsimile. It binds to folate receptor alpha (FRα), which is expressed in more than 90% of ovarian cancers, and can be illuminated using near-infrared light.
 Dr. Andrew D. Newton.
Dr. Andrew D. Newton."Ovarian cancer, as well as pulmonary carcinomas, are two of the cancers that we know of that have the highest levels of folate receptor alpha," study co-author Dr. Andrew D. Newton, a fifth-year surgery resident at Penn, told AuntMinnie.com. "This agent targets the folate receptor alpha, and we have taken advantage of this research."
OTL38 has also been used by Dr. Alexander Vahrmeijer, PhD, of Leiden University Medical Center in the Netherlands. Vahrmeijer and colleagues authored a 2016 study that confirmed that OTL38 accumulates in FRα-positive tumors and metastases. With near-infrared light illuminating the OTL38 agent, surgeons were able to remove an additional 29% of malignant lesions that could not be identified visually or palpated.
"Surgically removing tumors still leads to the best outcomes in cancer patients, and this study shows intraoperative molecular imaging can improve the surgeries themselves," Predina added. "The more we can improve surgeries, the better the outcomes for these patients will be."
In the U.S., On Target Laboratories of West Fayette, IN, manufactures OTL38, which is not yet commercially available. The company develops small molecules that target and illuminate specific cancerous cells and other diseased tissue when combined with fluorescent dyes.
Preoperative imaging
For this study, the Penn researchers enrolled 50 subjects (35 males, 15 females; mean age of 67 years ± 9.8 years) between July 2015 and November 2016. The patients had resectable pulmonary nodules identified by CT that were either suspected or confirmed to be malignant with histology. Subjects also underwent a preoperative PET/CT scan within 30 days of pulmonary resection. A standardized uptake value (SUV) of greater than 2.0 for FDG was considered a positive lesion.
Preoperative PET/CT discovered a total of 66 pulmonary nodules, with a mean of 1.3 nodules per subject. Among the subjects, there were 39 (78%) patients with a single solitary pulmonary nodule, 11 (22%) subjects with multiple suspicious nodules, and eight (16%) cases with two pulmonary nodules.
Of the 66 nodules, 56 nodules (85%) were positive (SUVmean of 6.5 ± 3.7), compared with 10 nodules (15%) that were not FDG-avid (SUVmean of 1.2 ± 0.3).
IMI discoveries
Participants also intravenously received 0.025 mg/kg of OTL38 three to six hours before resection. When it came time for the resection, clinicians used the fluorescence of the nodules as part of the intraoperative molecular imaging and surgical procedure. Real-time fluorescent imaging was done with a high-definition camera that could emit and detect light in the near-infrared spectrum, thus detecting OTL38.
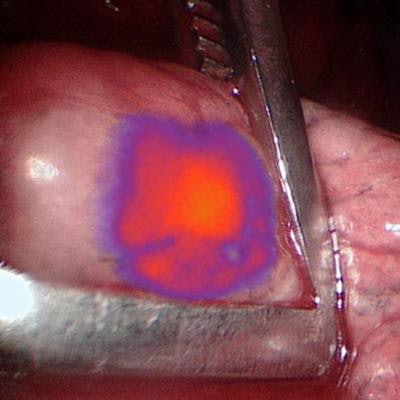
During the operation, the intraoperative molecular imaging technique with OTL38 identified 60 (91%) of the 66 pulmonary nodules detected with preoperative imaging. IMI with OTL38 also detected nine additional malignant lesions that were not seen on preoperative scans. The findings prompted clinically upstaging for six (12%) of the 50 patients and altered the care management for 15 (30%) subjects.
"This was a somewhat serendipitous find. We actually envisioned these initial patients as a proof of concept," Predina told AuntMinnie.com. "But we found when we looked at the first 50 patients we had enrolled, [IMI with OTL38] not only found lung cancers that we already knew about, but it also helped us find disease that, quite frankly, we probably would've never found in the operating room."
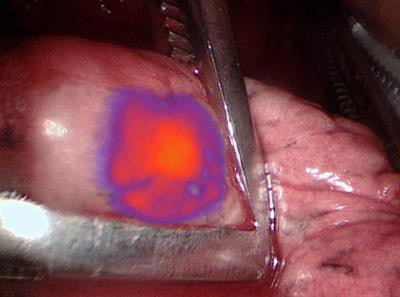 IMI with OTL38 illuminates lung nodules seen on PET/CT to give surgeons a better view. Image courtesy of Dr. Jarrod Predina et al and University of Pennsylvania Perelman School of Medicine.
IMI with OTL38 illuminates lung nodules seen on PET/CT to give surgeons a better view. Image courtesy of Dr. Jarrod Predina et al and University of Pennsylvania Perelman School of Medicine.Based on the total number of 75 nodules seen by the two modalities, intraoperative molecular imaging was more accurate by detecting 68 nodules (91%), compared with 51 nodules (68%) seen on PET. Thus, sensitivity for IMI (95.6%) outpaced PET (73.5%) (p = 0.001), and IMI also achieved greater positive predictive values (94.2%), compared with PET (89.3%) (p > 0.05).
IMI with OTL38 also was able to identify nodules as small as 0.5 cm, compared with preoperatively detected nodules of 2.4 cm by PET/CT (p < 0.01), even though fluorescence was similar in both situation (tumor-to-background ratio 3.3 and 3.1, respectively; p = 0.50).
"OTL38 seems to do an excellent job of not only characterizing those nodules that were identified preoperatively, but also helping to characterize and identify nodules that are below the threshold of PET detection," Predina said. "So we are able to find a number of nodules even down to the 1-mm range."
Promising technique
Penn researchers currently are in the early stages of a phase II study to validate and replicate this study's results. They have added Beth Israel Deaconess Medical Center at Harvard University in Boston, the University of Pittsburgh, and MD Anderson Cancer Center in Houston as research contributors with a goal to increase the cohort to at least 120 subjects.
"One of the nice things about the phase II is that it will help confirm that these results are reproducible and also help determine if these results are generalizable to clinicians who do not have exposure to molecular imaging," said Predina, who also is a surgical resident at Massachusetts General Hospital in Boston. "What we are finding is that this technique is confirming our results at these other institutions, which are beginning to see similar results. That is very encouraging."
One test will be to see how radiologists and clinicians adapt to intraoperative molecular imaging with OTL38. Newton believes that it will become more commonplace over time and with more experience.
"I think the technology itself is not that hard to use, especially for surgeons who are used to having devices in the OR," Newton said. "The hard part is interpreting the results. The first time you see it, sometimes there is some fluorescence in the background. It could take several times to get to know what is normal."