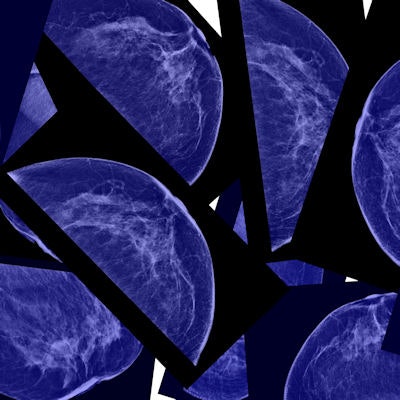
One of the more controversial ideas advanced by some critics of screening mammography is that it finds cancers that might "spontaneously regress" -- that is, disappear on their own. But that belief is being refuted by a new study published online April 27 in the Journal of the American College of Radiology.
The new findings indicate that cancers detected at mammography don't disappear; they just show up at the next screening round, whenever it occurs.
"Despite the benefit of decreased breast cancer-specific mortality associated with screening mammography, aggressive attempts to limit screening have been made by some who value the reported 'harms' of screening more than the proven mortality benefit," wrote a team led by Dr. Elizabeth Kagan Arleo of NewYork-Presbyterian. "[But] in our experience, untreated breast cancer does not spontaneously disappear or regress, so those screening-detected cancers that involve overdiagnosis will be detected, diagnosed, and treated whenever the next screening examination is done."
Skeptical science?
Recent articles about mammography screening have claimed that breast cancers can spontaneously regress and disappear. But this spontaneous regression idea is wrong, corresponding author Dr. Debra Monticciolo of Texas A&M University and Scott & White Medical Center in Temple, TX, told AuntMinnie.com.
 Dr. Debra Monticciolo from Texas A&M University.
Dr. Debra Monticciolo from Texas A&M University."Those of us who work with breast cancer diagnosis were skeptical of this claim, so we chose to approach it scientifically," she said. "Our research directly refutes the [U.S. Preventive Services Task Force's] claim that waiting until age 50, or screening every other year instead of every year, will decrease the small amount of overdiagnosis that exists."
Arleo and colleagues sought to investigate the spontaneous regression argument with a survey of 42 Society of Breast Imaging fellows conducted in December 2016, asking them to report outcomes data from their screening mammography practices. The average number of screening mammograms read in each practice in the past 12 months was 25,203; the average number of screening mammograms interpreted over the past decade was 228,844.
Among all practices, 25,281 screen-detected invasive breast cancers and 9,360 screen-detected ductal carcinomas in situ (DCIS) were reported over the past decade. These included 240 cases of untreated invasive breast cancer and 239 cases of untreated DCIS. None of the cancers spontaneously disappeared or regressed at the next mammography exam.
What's the takeaway? Overdiagnosis should not be a factor in setting screening intervals, according to the researchers. In other words, an "overdiagnosed" cancer will appear suspicious for malignancy on imaging regardless of the age at initial screening or screening interval, Arleo and colleagues noted. So starting screening at a later age -- at 45 or 50 instead of 40 -- and increasing the screening interval from annual to biennial just delays the timing of overdiagnosis without decreasing the frequency of it, they wrote.
"Our result, that the frequency of screen-detected breast cancers that spontaneously disappear or regress is zero, supports the argument that overdiagnosis should not be considered in the decision regarding whether to screen more (start screening at an earlier age, screen at a shorter interval) or screen less," the group wrote.
Spontaneous regression?
The study findings don't challenge the existence of overdiagnosis, the authors wrote. Rather, they show that all untreated, screen-detected cancers persist and remain suspicious for malignancy.
"Therefore, reducing the frequency of screening will not reduce the frequency of overdiagnosis because what might have been in a screening examination that is part of a 'more frequent' screening regimen will still be overdiagnosed at the next screening examination that is part of a 'less frequent' screening regimen," they wrote.
So if a woman chooses to be screened less frequently, or at a later age, and she has a screening-detected, overdiagnosed lesion with no negative effect on her health -- compared to earlier detection under a protocol of more screening -- what is lost? If it could be guaranteed that her health would not be negatively affected, nothing is lost. But that's the problem, according to the group.
"We currently do not know which screen-detected cancers are so indolent as to have no health decrement if they would be detected, diagnosed, and treated later, versus which screen-detected cancers are progressive and hence would grow to larger size, node positivity, and more advanced stage, with corresponding increases in the risk for premature death of breast cancer as well as more aggressive and toxic cancer therapy," the authors wrote.
The bottom line is that overdiagnosis is not mitigated by later-onset or less-frequent screening, according to Monticciolo.
"Screening saves lives," she said. "We need to find breast cancers at the earliest stage possible, and we hope this research will further stimulate physicians of all types to help us in the battle against breast cancer by encouraging women to have yearly mammograms starting at age 40."