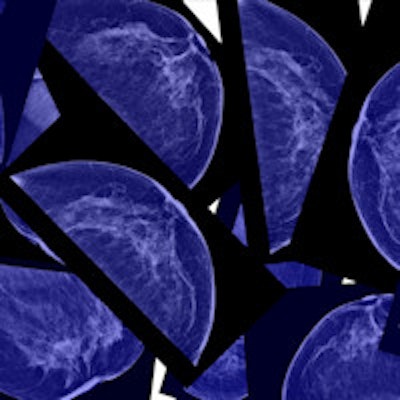
A study of nearly 2,000 breast cancer patients who underwent screening mammography found significant differences between three different methods of measuring breast density -- though breast cancer risk predictions were similar among the techniques, concludes a report in Radiology.
Study participants underwent digital mammography at the Mayo Clinic in Rochester, MN, or at one of four sites in San Francisco between 2006 and 2012. The scans were examined on average more than a year before cancer diagnosis using one of three methods: one in which a radiologist visually determined density based on BI-RADS breast density classifications, and two in which automated breast density measurements were derived from software from one of two vendors, Volpara Health Technologies or Hologic.
The results varied considerably between the techniques, showing a 14% divergence between the automated scans and the BI-RADS density classifications. Between 37% and 51% of participants were classified as having dense breasts, depending on the method used to measure density. A measure of dense-breast volume known as volumetric percentage density differed the least among the three techniques.
"These differences have implications for the numbers of women who have discussions with providers about supplemental screening," wrote Dr. Kathleen Brandt from the Mayo Clinic, along with colleagues from Mayo, the University of New Mexico, and the University of California, San Francisco (Radiology, December 22, 2015).
Risk in dense breasts
Dense breasts are a major risk factor for the development of breast cancer, and density is inversely related to the sensitivity of mammography, the authors noted. Dense breasts are relatively common, although density patterns vary widely.
The BI-RADS density classification system consists of four categories of increasing density. About 40% of women have scattered fibroglandular densities, categorized as BI-RADS 2; another 45% have heterogeneously dense breasts, categorized as BI-RADS 3; and 6% have extremely dense breasts, categorized as BI-RADS 4. Together, these represent about half of the female population in the U.S.
In addition to the BI-RADS system, there are two commercially available automated density measurement methods for digital mammography studies, Volpara and Quantra (Hologic).
Women with dense breasts at mammography are advised to discuss supplemental screening with their doctors, so the distinction is important. But how much does the characterization of breast tissue depend on the method used to determine it?
To find out, the researchers looked at 1,911 patients with breast cancer and 4,170 control subjects, matched for age, race, exam data, and mammography equipment, who underwent mammography at one of five sites between 2006 and 2012. The data were analyzed for breast density using the three methods at a mean 2.1 years before cancer diagnosis (range, 6 months to 6 years), and the level of agreement between the techniques was determined.
Methods yield different assessments
Nearly three-fourths (72%) of the cases were invasive cancer, and patients with breast cancer were more likely than control subjects to have higher breast density by all assessment methods, the authors wrote.
The results showed only moderate agreement between clinical BI-RADS density classifications and the Volpara and Quantra BI-RADS estimates.
Overall, the analysis revealed differences as high as 14% between the three methods in the proportion of women having dense breasts, with Volpara classifying 51% as having dense breasts, Quantra classifying 37%, and clinical BI-RADS classifying 43%.
"These differences have implications for the numbers of women who have discussions with providers about supplemental screening," Brandt and colleagues wrote. "We also found Volpara and Quantra automated density methods to be positively associated with future breast cancer risk."
The group calculated the odds ratio that a cancer diagnosis was linked to how each method classified women as BI-RADS 2.
| Density associations with breast cancer diagnosis | ||
| Method | Odds ratio | 95% confidence interval |
| Volpara | 1.8 | 1.5-2.2 |
| Quantra | 1.9 | 1.5-2.5 |
| Clinical BI-RADS | 2.3 | 1.9-2.8 |
In assessing different metrics used by the automated methods, the association with breast cancer risk was stronger using volumetric percentage density (VPD) than dense volume (DV), "which suggests that this metric is more appropriate in clinical practice for risk assessment," the authors noted.
Median VPD was 7.7% for Volpara and 10.1% for Quantra, with similar interquartile ranges. Volpara showed more women with low VPD than Quantra, but a similar proportion had extremely high VPD.
For its part, clinical BI-RADS assessment showed better discrimination of case status (C = 0.60) than either of the automated methods (Volpara, C = 0.58; Quantra, C = 0.56).
Thus, although clinical BI-RADS density can be used to identify women at high risk of interval cancer, the ability of automated methods to predict the risk of interval cancer is not yet known, according to the authors.
The method used to define dense breasts "could have a substantial effect on practice patterns," they wrote. "Second, on the basis of results from our study, it would be essential to use the same automated density measurement method to assess individual longitudinal changes This will be especially important if breast density is used as a surrogate marker for treatment response."