Imaging volume per Medicare beneficiary decreased by 3.2% from 2011 to 2012, but the use of imaging services has remained much higher than it was a decade ago, according to the Medicare Payment Advisory Commission's (MedPAC) annual report to Congress.
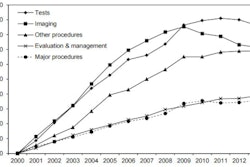
The agency recognized the decline in Medicare imaging volume in a report it released on March 14, but it focused on the fact that overall cumulative growth in imaging volume from 2000 to 2009 totaled 85%, compared with a cumulative decrease in imaging volume since then of about 7%.
"Despite decreases after 2009, use of imaging services has remained much higher than it was a decade ago," MedPAC wrote in its 2014 "Report to the Congress: Medicare Payment Policy."
"The growth in imaging volume from 2000 to 2009 was exceeded only by the 86% growth in the use of tests -- such as allergy tests -- during those years," according to the agency.
| Changes in Medicare imaging volume | |
| Average annual change in units of service per beneficiary, 2007-2011 | 0.6% |
| Change in units of service per beneficiary, 2011-2012 | -1.9% |
| Average change in volume per beneficiary, 2007-2011 | 0.2% |
| Change in volume per beneficiary, 2011-2012 | -3.2% |
| Percent of 2012 allowed charges | 11.9% |
The decrease in imaging volume is due in part to the shift in billing for cardiovascular imaging from physician offices to hospital outpatient departments, MedPAC found. In 2012 compared with 2011, the number of echocardiograms per beneficiary provided in hospital outpatient departments went up by 13.5%, but the number provided in professional offices decreased by 9%.
In addition, from 2011 to 2012, the number of cardiac nuclear medicine studies per beneficiary provided in hospital outpatient departments increased by 9.4%, while the number provided in professional offices decreased by 15.9%. These changes in billing patterns are consistent with reports of an increase in hospital-owned cardiologist practices, the agency wrote.
"Some of the 3.2% decrease in the volume of imaging services results from decreases in units of service for nuclear medicine and echocardiography," MedPAC wrote. "However, the most important factor is the movement of these services from the nonfacility setting to the facility setting. If these two types of services are excluded from the calculations, the volume of all other imaging services from 2011 through 2012 would show a decrease of 1.9% instead of 3.2%."
SGR repeal is of highest priority
In its report, MedPAC reiterated its long-standing recommendation to repeal the sustainable growth rate (SGR) formula. After a decade of year-end legislative overrides, the policy is causing uncertainty for physician and other clinician practices and has the potential to create instability for beneficiaries.
"MedPAC's highest policy priority with respect to Medicare's payments to physicians and other health professionals is repeal of the SGR," the commission wrote.
MedPAC suggested that Congress take the following four actions:
- Repeal the SGR and replace it with 10 years of legislated updates. Updated percentages would differ for clinicians who deliver primary care and those who deliver other services: Fees for nonprimary care services would be reduced by less than 3% in each of the first three years, followed by a freeze, while fees for primary care would be frozen for 10 years. This way, physicians would shoulder about one-third of the cost of repealing the SGR, according to MedPAC.
- Collect data to improve the relative valuation of services. The commission is recommending that the Secretary of the Department of Health and Human Services regularly collect data -- including service volume and work time -- to establish more accurate work and practice expense values.
- Identify overpriced services and rebalance payments.
- Encourage accountable care organizations (ACOs) by creating greater opportunities for shared savings. Physicians who join or lead two-sided risk ACOs should be afforded a greater opportunity for shared savings than those in bonus-only ACOs and those who do not join any ACO, according to MedPAC.
"Repeal of the SGR should be done in a fiscally responsible way," MedPAC wrote. "The commission's recommendations to the Congress aim to preserve or enhance beneficiary access to quality care, while minimizing the financial burden on beneficiaries and taxpayers."