An augmented reality image overlay system can provide accurate and efficient MR guidance of shoulder and hip arthrography procedures, possibly combining joint injection and MRI into a single procedure, according to research published online in Radiology.
Using an augmented reality prototype in conjunction with a 1.5-tesla MR scanner in 45 arthrography procedures on cadavers, a research team led by Dr. Jan Fritz of Johns Hopkins University School of Medicine found that the image overlay technology effectively guided the injections in all procedures, with no statistical differences in operator performance.
"Image overlay technology combines joint injection and MR imaging into a single procedure, thereby avoiding a more complex scheduling process, possible exposure to ionizing radiation, and the need for an additional co-located modality," the authors wrote. "The availability of image overlay navigation allows performance of procedures at outpatient imaging centers without access to a fluoroscopy unit and can obviate CT guidance for joint injections."
While fluoroscopy and CT guidance come with exposure to ionizing radiation, interventional MRI can combine joint injection and MRI in a single setting. However, this usually requires targeting and puncture inside the magnet bore, according to the authors.
Outside the bore
Because augmented reality navigation technology can facilitate MRI-guided targeting and puncture outside the bore, the authors sought to determine if this overlay technology could effectively provide targeting for MR-guided shoulder and hip joint arthrography (Radiology, July 27, 2012).
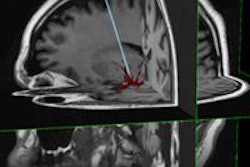
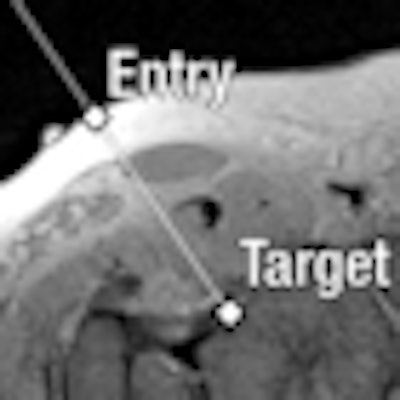
The Perk Station prototype, used with a Magnetom Espree 1.5-tesla scanner (Siemens Healthcare), plans virtual needle paths on MR images of the target joint with version 3.6 of the 3D Slicer software. An MR image with the virtual needle path is then projected onto the subject, and an operator punctures the joint by maneuvering the actual needle along the virtual path, according to the researchers.
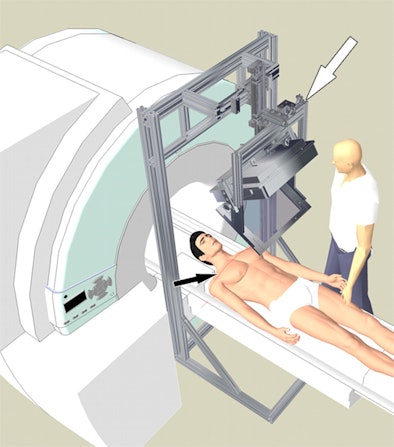 |
| Schematic of interventional setup of prototype augmented reality image overlay system (white arrow) in conjunction with a clinical 1.5-tesla MR scanner. The red laser line (black arrow) on the subject's skin coincides with the selected MR image target. All images courtesy of Radiology. |
Two operators performed 45 arthrography procedures, including 23 shoulders and 22 hips. Operator A performed 12 shoulder and 12 hip injections, while operator B handled 11 shoulder and 10 hip injections. Each operator performed procedures on different cadavers using the image overlay guidance prototype.
MRI was employed to confirm needle positions, monitor injections, and perform MR arthrography, according to Fritz and colleagues. They then assessed accuracy based on the rate of needle adjustment, target error, and whether the injection was intra-articular. Arthrography procedural time served as the efficiency measure.
Needle adjustment was required in six (13%) of the procedures; once for operator A and five times for operator B. Target error was 3.1 mm ± 1.2; operator A had a target error of 2.9 mm ± 1.4, while operator B had a target error of 3.5 mm ± 0.9. Intra-articular injection was successful in all 45 cases.
"Our investigation demonstrated that [augmented reality] image overlay technology provides accurate MR imaging guidance for intra-articular injection of contrast material into shoulder and hip joints," the authors wrote.
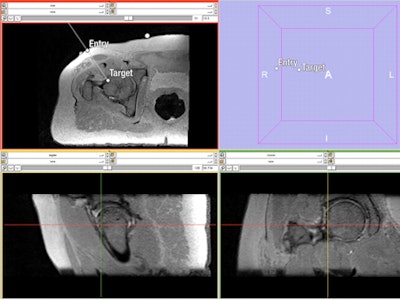 |
| Needle path planning to the femoral head-neck junction with 3D sampling perfection with application optimized contrast using different flip angle evolutions (SPACE) MRI sequence. Axial reformation is shown on the top left, while a 3D map is on the top right. A sagittal reformation is presented on the bottom left, and a coronal reformation is on the bottom right. |
Efficiency and reliability
The average arthrography procedure time was 14 minutes, with a range of six to 27 minutes. Operator A had an average time of 12 minutes, with a range of six to 25 minutes, while operator B had an average time of 16 minutes, with a range of six to 27 minutes. The operator differences were not significant for needle adjustment rate (p = 0.08), target error (p = 0.07), intra-articular injection rate (p < 0.99), or arthrography time (p = 0.22).
"This [augmented reality] technique has the potential to simplify the workflow of direct MR arthrography in patients by combining joint injection and diagnostic high-field-strength MR imaging into a single procedure, while avoiding exposure to ionizing radiation of patients and operators," the authors wrote.
The researchers plan to assess the method's technical efficacy in an upcoming clinical trial.