New research from Germany shows how cardiac MRI (CMR) can assess myocardial function by combining cine imaging, stress perfusion, and scar imaging to produce a high percentage of correct diagnoses and high-quality images, according to results published January 25 in the Journal of the American College of Cardiology.
The findings are important because a reliable high-resolution MRI technique could compete with stress SPECT myocardial perfusion imaging, the current method of choice for diagnosing and predicting outcomes in patients with suspected or known coronary artery disease (CAD). In SPECT imaging, a semiquantitative segmental system is used to estimate the ischemic burden at stress and rest, and gauge the extent and severity of reversible defects. But a radiation-free way to determine myocardial ischemic burden of the entire heart is desirable, and 3D cardiac MRI stress perfusion imaging could fill this need.
The technique achieves faster dynamic imaging by means of reduced data acquisition on the basis of exploiting correlations in k-space and time, wrote Robert Manka, MD, and colleagues from the German Heart Institute in Berlin and the University of Zurich in Switzerland. This provides full coverage of the heart while preserving adequate temporal and spatial resolution (JACC, January 25, 2011, Vol. 57:4, pp. 437-444).
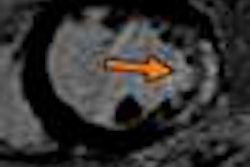
A recently introduced imaging technique known as k-t accelerated multislice cardiac MR provides information on the presence and transmurality of myocardial regional hypoperfusion with high in-plane spatial resolution, the authors wrote. Taking the technique a step further, the authors said that dynamic 3D perfusion MRI with preserved high in-plane resolution could permit direct volumetric measurements of myocardial hypoenhancement (volumehypo) without extrapolating the distribution of hypoperfused regions.
"The objective of this study was to determine the value of dynamic 3D-CMR perfusion imaging for the detection of CAD and volumetry of myocardial hypoenhancement before and after percutaneous coronary stenting," wrote Manka and colleagues.
The study examined 146 patients with known or suspected coronary artery disease who were referred for clinically indicated invasive coronary angiography. Patients were referred to coronary CT angiography for:
- Evaluation of chest pain syndromes or dyspnea
- Positive electrocardiography exams
- Cardiac risk stratification before noncardiac surgery
Cardiac MRI was performed on a 3-tesla scanner (Achieva 3.0T, Philips Healthcare, Andover, MA) equipped with a Quasar Dual gradient system and Philips software release 2.6.3. A.
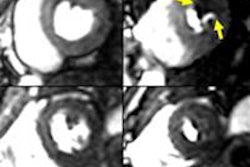
The cardiac MR exam included cine imaging, as well as 3D cardiac MR perfusion under adenosine stress and at rest, followed by delayed-enhancement imaging. Significant CAD was defined as greater than 50% luminal narrowing at invasive coronary angiography, while 3D-CMR perfusion scans were visually classified as pathologic if one segment or more showed an inducible perfusion deficit in the absence of delayed enhancement. Forty-eight patientsunderwent repeat cardiac MRI exams after percutaneous stenting. Volumehypo was measured by segmentation of the area of induciblehypoenhancement and normalized to left-ventricular myocardial volume (%volumehypo).
Image quality for rest and stress 3D-CMR perfusion was graded on a scale of 1 to 4, with 1 being nondiagnostic; image artifacts were noted and classified as breathing-related or k-t reconstruction-related, seen in image flickering. The 3D-CMR perfusion examinations were analyzed by an observer who was fully blinded to the clinical and angiographic patient data, Manka and his team wrote.
Three-dimensional cardiac MR perfusion imaging delivered sensitivity, specificity, and diagnostic accuracy of 91.7%, 74.3%, and 82.9%, respectively. Before and after coronary stenting, the %volumehypo averages were 14.2 ± 9.5% and 3.2 ± 5.2%, respectively, with a relative volumehypo reduction of 79.4 ± 25.4%. Intrareader and inter-reader reproducibility of volumehypo measurements was high.
The study is the first to assess the diagnostic value of dynamic 3D-CMR stress perfusion imaging for detecting CAD in patients with suspected or known coronary disease and to apply volumetric measurement of myocardial hypoenhancement before and after percutaneous coronary stenting, the authors wrote.
The impetus for developing dynamic 3D-CMR stress perfusion has been to ensure comprehensive coverage of the heart to improve diagnostic accuracy for detecting ischemic myocardial regions, and to allow for direct volumetric quantification of left-ventricular myocardial hypoenhancement, they explained.
"In patients with known or suspected CAD, dynamic 3D-CMR stress perfusion yielded high diagnostic accuracy for the detection of significant CAD," Manka and colleagues wrote. "Volumetry of myocardial hypoenhancement was highly reproducible and allowed for the assessment of the treatment effect achievable by percutaneous coronary stenting. Consequently, dynamic 3D-CMR stress perfusion imaging can be regarded as a powerful, noninvasive diagnostic tool for the detection and serial quantification of myocardial perfusion abnormalities during follow-up of anti-ischemic therapies."
By Eric Barnes
AuntMinnie.com staff writer
January 25, 2011
Related Reading
Normal whole-heart coronary MRA rules out significant coronary artery disease, September 28, 2010
3-tesla 3D cardiac MRI boosts therapy planning, September 23, 2010
CT, MRI look at different etiologies for myocardial fat, September 25, 2009
New 3D cardiac MRI tool helps preplan pediatric surgery, August 12, 2009
MR-IMPACT trial: CMR equivalent to SPECT for stenosis detection, February 18, 2008
Copyright © 2011 AuntMinnie.com