CHICAGO - Hepatocellular carcinoma (HCC) is characterized by highly vascular tumors that progress rapidly yet quite variably from patient to patient. In a new study, researchers are attempting to determine whether perfusion imaging can be used to assess the prognosis of the individual patient, and perhaps help direct treatment.
In a study presented today in an HCC session at the RSNA meeting, a team from Massachusetts General Hospital in Boston used CT perfusion to assess the vascularity of primary and metastatic HCC.
CT perfusion imaging has been used to study vascularity and monitor treatment response in various body tumors, said Dr. Nagaraj Holalkere in his talk.
"Our focus in this study was to assess the feasibility of using perfusion imaging to compare tumor vascularity in advanced HCC, compare perfusion parameters, and to see if there was any difference between the tumor and the background liver in terms of portal vein invasion and the presence or absence of cirrhosis, and to correlate the clinical markers of HCC with imaging findings," he said.
Thirty patients (21 men and 9 women; mean age 60), including 25 with advanced HCC (stages T3 and T4) and five with extrahepatic masses from HCC, underwent CT perfusion imaging. All cases were confirmed with biopsy. The exam was repeated in four patients within 24 hours to test the reproducibility of the exam.
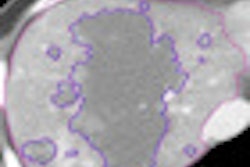
"Initially we acquired nonenhanced CT to localize the tumor, and we selected four contiguous slices of 5-mm thickness at the maximum diameter of the tumor, and we studied them with dynamic CT perfusion," Holalkere said.
All patients underwent CT perfusion imaging on a 16-detector scanner using dynamic first-pass CT with a breath-hold of 25 seconds at a static table position, following injection of 70 mL of nonionic contrast medium at 7 cc/sec and a five-second delay.
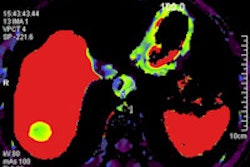
The images were interpreted at a workstation using GE CT Perfusion 2.0 software (GE Healthcare, Chalfont St. Giles, U.K.). Perfusion maps were generated to depict blood flow, blood volume, mean transit time, and permeability surface area product, Holalkere said.
CT perfusion parameters were correlated with tumor grades, angioinvasive disease, or cirrhosis, as well as the background liver, spleen, and extrahepatic metastases and clinical markers (alpha-fetoprotein and circulating endothelial cell levels) of HCC.
The group found significant differences in CT perfusion parameters between primary HCC and background liver.
"We obtained a very good correlation of CT perfusion parameters on repeat examination, with a correlation coefficient of 0.9 (p ≤ 0.05)," Holalkere said.
Overall perfusion variability was 4%; the least variable parameter was blood flow and the most variable parameter was permeability surface area product at 13%.
"When we compared the CT perfusion parameters among different grades (of HCC), we observed very high blood flow in well-differentiated tumors, as well as blood volume and permeability surface, and low mean transit time in well-differentiated tumors, as compared to moderately differentiated and poorly differentiated tumors (p ≤ 0.05)," he said. "However, there were no significant differences between (moderately) and poorly differentiated tumors."
No differences were seen between tumors with or without angioinvasion or cirrhosis; however, the background liver showed increased blood flow in patients with angioinvasion. Alpha-fetoprotein levels were highly variable. Lymph node metastases showed low perfusion levels compared to metastases at other sites. CT perfusion parameters did not correlate with clinical markers for HCC.
Pointing to an image of a patient with portal-venous invasion of the HCC tumor, Holalkere noted: "We didn't observe any differences in the perfusion parameters of the tumor; however, we obtained a very high blood flow in the background liver … which we believe could be due to portal-venous shunting."
Finally, the group observed relatively high perfusion parameters in peritoneal, lung, and bone metastases, similar to the primary HCC, whereas lymph node metastases demonstrated very low perfusion parameters.
"CT perfusion is a feasible and reproducible technique, and we demonstrated distinct perfusion parameters in well-differentiated HCC, background liver in the presence of portal vein invasion, and low perfusion parameters in lymph node metastases," Holalkere concluded. "However, there was no correlation of CT perfusion parameters with clinical markers."
By Eric Barnes
AuntMinnie.com staff writer
November 29, 2005
Related Reading
Iodine-131 lipiodol offers palliation in hepatocellular carcinoma, October 13, 2005
Radiofrequency ablation better than ethanol injection for small liver cancers, August 10, 2005
Early arterial phase best for HCC detection, December 28, 2004
Copyright © 2004 AuntMinnie.com