Acute Chest Syndrome of Sickle Cell:
Clinical:
Acute chest syndrome (ACS) is a potentially life threatening complication of sickle cell disease. ACS is defined as a pulmonary illness with fever, chest pain, leukocytosis, and a new pulmonary opacity on a chest radiograph in a patient with sickle cell disease [2]. It has been estimated that 50% of all sickle cell patients will have at least on episode of ACS in their lifetime [2] and up to 25% of deaths of sickle cell patients can be attributable to ACS. The syndrome is postulated to occur secondary to microvascular occlusion/thrombosis within the pulmonary vasculature with subsequent infarction. The pulmonary arterial bed has low oxygen tension which facilitates polymerization of hemoglobin S. Repeated episodes of ACS lead to pulmonary arterial hypertension and cor pulmonale. Underlying pulmonary infection (pneumonia) has been implicated as an inciting etiology for ACS, however, the true incidence of infection may be much less than previously suspected. Affected patients present with chest pain, fever, hypoxia, leukocytosis, and prostration- thus, on clinical exam, differentiation between ACS and pneumonia is rarely possible during an acute episode. Treatment of ACS involves intravenous hydration, analgesics, and broad spectrum antibiotics. Partial exchange transfusions are used for the treatment of severe ACS (PaO2 levels below 70 mm Hg). Rapid clinical and radiographic improvement can be seen following transfusion therapy [2].X-ray:
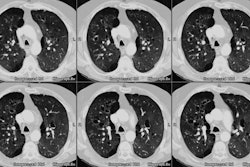
Radiographs: The CXR very commonly demonstrates segmental or lobar areas of parenchymal consolidation which likely reflect areas of parenchymal infarction. Multiple lobes can be involved in nearly half of the patients. Pleural effusions can be found in up to 68% of cases (bilateral in 37%). Radiographically, the findings are indistinguishable from pneumonia.Computed Tomography: On CT, the key to the diagnosis of ACS is the presence of areas of hypoperfusion characterized by decreased or absent small vascular markings. Areas of ground glass attenuation are common- they can be geographic, patchy, or lobar. Areas of ground glass attenuation tend to be located in regions of decreased vascularity and may represent hemorrhagic edema due to parenchymal ischemic damage. Areas of frank consolidation can be found in up to 100% of cases and likely represent parenchymal infarction, but these can be difficult to distinguish from bacterial pneumonia. Chronic changes are seen in individuals with repeated acute episodes, with approximately half showing evidence of interstitial disease, most probably reflecting scarring from small pulmonary infarcts [4].
REFERENCES:
(2) Pediatr Radiol 1997 Aug;27(8):637-641
(3) J Thorac Imaging 1998; Leong CS, et al. Thoracic manifestations of sickle cell disease. 13: 128-134
(4) Radiology 2002; Hansell DM, et al. Small-vessel diseases of the lung: CT-pathologic correlates. 225: 639-653