Hemoptysis:
Clinical:
The most common cause of hemoptysis is bronchiectasis, however, other etiologies such as malignancy, tuberculosis, aspergillosis, bronchitis, and congenital cardiac or pulmonary vascular anomlies may also produce hemoptysis [2,5]. Despite thorough evaluation, an etiology for hemoptysis may not be detected in nearly 20% of cases which is referred to as "cryptogenic" hemoptysis [9]. About 5% of patients that present with hemoptysis and a negative CXR are found to have lung cancer. Up to 10% of smokers who present with cryptogenic hemoptysis will develop a lung cancer within the next 3 years [9]. CT scanning has been shown to be more sensitive than bronchoscopy in determining the etiology of hemoptysis [1].Massive hemoptysis is defined as the expectoration of more than 300 ml of blood in 24 hours. However, a more appropriate definition might be any volume of expectorated blood that is life-threatening by virtue of airway obstruction, hypotension, or blood loss [3]. Patients with massive hemoptysis have a high mortality (up to 35% in surgically treated patients and 50-100% with conservative management) [2,7]. The cause of death is usually due to asphyxiation from flooding of the airways with blood, rather than from exsanguination [2]. The bronchial arteries are the source of bleeding in most cases [4]. Physiologic factors which contribute to massive hemoptysis include development of enlarged and tortuous bronchial arteries adjacent to areas of inflammation, erosion of blood vessels, formation of bronchopulmonary arterial fistulae, and pulmonary hypertension. Pulmonary artery pseudoaneurysms are the main cause of bleeding from the pulmonary arteries and can occur secondary to blunt or penetrating trauma, iatrogenic trauma from central lines, neoplasm, lung abscess or inflammatory condition [6]. The mortality rate associated with a PAP is as high as 50% [6]. The incidence of PAP in patients with massive hemoptysis has been reported to be between 5-11% [6].
Bronchial artery embolization is a well accepted procedure for the management of massive hemoptysis [5]. The bronchial arteries originate from the thoracic aorta between the T3 and T7 vertebrae (usually between T5 and T6). Prior to embolization, careful attention must be paid to the opacification of a spinal artery that may also arise from an intercostal artery- the presence of a spinal artery is a relative contraindication to therapeutic embolization [2]. Transcatheter embolization can control acute bleeding in 86% to 98% of cases, but recurrent bleeding occurs in 10-50% of cases [2]. This is to be expected as the embolization does not treat the underlying condition which precipitated the bleeding. Complications of bronchial artery embolization include post embolization syndrome (chest pain, fever, leukocytosis, and dysphagia) which can last 5 to 7 days, bronchial devascularization which can lead to bronchial stenosis, and ischemic myelitis with subsequent paralysis [2].
X-ray:
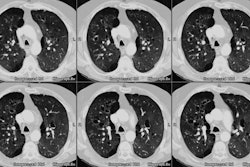
Helical CT: For patients presenting with hemoptysis and a non-localizing CXR, in addition to detecting bronchiectasis, the CT scan should be used to exclude an occult central or endobronchial lesion. An initial sequence of 7 mm scans with a pitch of 1 obtained from the apex to the carina, followed by 3-5 mm sections with a pitch of 1 to 1.6 from the carina through the inferior pulmonary veins, and then 1-2 mm sections every 10 mm to the bases is an adequate approach.A bronchial artery with a diameter of greater than 2 mm is considered to be abnormal and may be a source of hemoptysis [5]. Extravasation of contrast material is very specific for the site of bronchial bleeding, but is seen in only 4-11% of cases [5].
REFERENCES:
(1) Chest 1994; 105: p.1155-1162
(2) J Thorac Imaging 1998; Najarian KE, et al. Arterial embolization in the chest. 13: 93-104
(3) AJR 2001; Hsiao EI, et al. Utility of fiber optic bronchoscopy before bronchial artery embolization for massive hemoptysis. 177: 861-867
(4) Radiographics 2006; Bruzzi JF, et al. Multidetector row CT of hemoptysis. 26: 3-22
(5) AJR 2006; Chung MJ, et al. Bronchial and nonbronchial systemic arteries in patients with hemoptysis: depiction on MDCT angiography. 186: 649-655
(6) Radiology 2010; Shin S, et al. Peripheral pulmonary arterial
pseudoaneurysms: therapeutic implications of endovascular
treatment and angiographic classifications. 256: 656-664
(7) Radiographics 2015; Walker CM, et al. Bronchial arteries: anatomy, function, hypertrophy, and anomalies. 35: 32-49