Germ Cell Neoplasms:
View cases of germ cell neoplasms
Clinical:
The mediastinum is the most common extra-gonadal site for germ cell tumors [6] which account for about 1-15% of mediastinal masses in adults, and 25% in children [7]. The tumors are felt to develop from germ cell rests which remain in the mediastinum. The great majority of these lesions are benign (80%)- the most common being benign teratoma [7]. Benign lesions occur with equal frequency in men and women; but malignant mediastinal germ cell neoplasms are much more common in males (9:1), have a peak prevalence in the third decade of life, and typically have a poor prognosis [7]. The exception to this is mediastinal seminoma which is very radiosensitive and these patients have an overall survival rate of 75%. Calcification in malignant lesions is exceedingly rare (1%) [1].
Mediastinal Teratoma:
Clinical:
Teratomas are the most common germ cell tumors of the mediastinum, accounting for 60-80% of lesions. (Seminomas are less common, and usually discovered in males). Patients are usually less than 30 years of age. Histologically there are 3 types of teratomas:
i- Mature: Mediastinal mature teratoma is the most common primary germ cell tumors of the mediastinum accounting for about 75% of cases. It is a benign, slow growing lesion. Mature teratomas occur with equal frequency in males in females (although there may be a slight female predominance). Most patients are under the age of 40 years (Mean 24 years). Symptoms are found in 47% to 73% of patients- usually chest pain, dyspnea, or cough. Severe symptoms such as chest pain or hemoptysis are more commonly associated with ruptured tumors, although patients can be asymptomatic [4]. Tumor rupture is a serious and unique complication associated with mature mediastinal teratomas- possibly related to the production of proteolytic enzymes produced by glandular tissue within the lesion [4]. Alternatively, rapid tumor enlargement may result in ischemic change that leads to rupture [4]. Rupture can occur in up to 36% of all cases [3], most frequently into the lung and bronchial tree, followed by the pleural or pericardial space. Rupture into the lung causes pneumonia, while rupture into the pleural space will produce a chemical pleuritis with a characteristic fat-fluid level.
ii- Immature: Histologically fetal tissue is seen within the lesions and there is a greater risk of malignancy.
iii- Teratoma with additional malignant components/Teratocarcinoma: Malignant teratomas occur more commonly in male patients. Metastatic spread commonly occurs to regional lymph nodes, liver, lungs, and bone.
X-ray:
On CXR, the lesion appears as a well circumscribed anterior mediastinal mass. Calcification can be seen in up to 26% of cases [5].
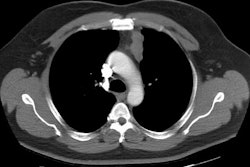
On CT benign lesions are typically well marginated, lobulated, encapsulated, mixed solid/cystic masses that arise in or near the thymus (anterior mediastinum). The lesion typically extends to one side of the midline. The lesion may extend into other mediastinal compartments in up to 13% of cases. Isolated posterior mediastinal lesions account for only 3% of cases. Fluid containing cystic areas are found in up to 88% of cases, are commonly mutlilocular (25%), and are separated by thin tissue septa. Lesions are predominantly cystic in 80% of cases. Other findings include fat within the lesion (50-73%), calcifications (up to 25-50% of benign lesions), and a fat-fluid layer (up to 11% of cases). Pleural effusion can be found in up to 17% of cases (pericardial effusion in 5%). [2] Ruptured lesions tend to have a heterogeneous internal architexture, are associated with consolidation/atelectasis/or fat containing masses in the ajacent lung, or have an associated pleural effusion [4].
Malignant lesions are poorly defined with irregular borders which infiltrate the mediastinal fat. Malignant teratomas also have more solid components, compress adjacent structures, have a thick enhancing capsule, and contain areas of necrosis or hemorrhage [7].
Seminoma: (Germinoma)
Seminoma is the second most common mediastinal germ cell tumor. Most patients are males between the ages of 20-40 years. About 1/3 of patients are asymptomatic. If symptoms are present they relate to the size of the lesion. HCG levels are elevated in 7-18% of patients (alpha feto-protein levels are not elevated). The lesion most commonly metastasizes to regional nodes, the lungs, and the bone. The neoplasm is very chemo/radiosensitive and five year survival rates greater than 75% are not uncommon.
On radiologic evaluation seminomas are usually large, well marginated, homogeneous soft tissue density anterior mediastinal masses. Slight enhancement is seen with contrast administration. Calcification is rare [5].
Non-seminomatous Malignant Germ Cell Tumors:
Embryonal carcinoma, endodermal sinus tumor, choriocarcinoma, and combinations of these histologic types constitute non-seminomatous germ cell tumors. These lesions affect men almost exclusively [5]. Approximately 20% of non-seminomatous malignant mediastinal germ cell tumors are associated with Klinefelter syndrome (47,XXY). Alpha-fetoprotein levels are elevated in 80% of patients and is associated with endodermal sinus tumor or embryonal cell carcinoma. HCG levels are elevated in 30% of patients. Combined XRT and chemotherapy is the treatment of choice and 5 year survival is about 50%. These patients are also at risk for developing a concurrent hematologic malignancy unrelated to chemotherapy.
On radiologic evaluation the tumors are usually large and contain large areas of hemorrhage and necrosis. The surrounding fat planes are typically obliterated.
REFERENCES:
(1) Radiographics 1992; 12:1013-1030
(3) AJR 1998; Sasaka K, et al. Spontaneous rupture: A complication of benign mature teratomas of the mediastinum. 170: 323-328 (No abstract available.)
(4) AJR 1998; Choi SJ, et al. Mediastinal teratoma: CT differentiation of ruptured and unruptured tumors. 171: 591-594
(5) J Thoracic Imag 1999; Strollo DC, et al. Tumors of the thymus. 14: 152-171
(6) Radiographics 2004; Ueno T, et al. Spectrum of germ cell tumors: from head to toe. 24: 387-404
(7) Radiographics 2010; Nasseri F, Eftekhari F. Clinical and radiologic review of the normal and abnormal thymus: pearls and pitfalls. 30: 413-428