Castleman's Disease:
Clinical:
Castleman's is an uncommon nonclonal lymphoproliferative disorder secondary to lymphoid follicle hyperplasia and marked capillary proliferation with endothelial hyperplasia. It is a reactive, rather than a neoplastic, disorder caused by an unidentified antigenic stimulus or faulty immunoregulation. Autoimmune diseases and diseases of immune dysregulation are associated with Castleman's disease including paraneoplastic pemphigus, myasthenia gravis, Wiskott-Aldrich syndrome, and POEMS syndrome (peripheral neuropathy, organomegaly, endocrinopathy, monoclonal M protein, and slin lesions) [14]. Although the histologic findings of the disorder are characteristic, they are non-specific as they have been reported to occur in other conditions including drug reactions, Sjogren's syndrome, and Hodgkin's disease [5]. Castlemans disease occurs most commonly in the thorax (64% to 70% of cases), but can also occur in the abdomen (10-15% of cases- most commonly the retroperitoneum), the neck (10-15% of cases), or axilla [6,9]. Extralymphatic sites of involvement include the lungs, larynx, parotid glands, pancreas, meninges, and muscles [11].Most commonly, Castleman is classified clinically as unicentric or multicentric [14]. There are 3 histologic forms: 1- Hyaline Vascular (generally localized/unicentric); 2- Plasma Cell Variant (generally multicentric); and 3- Human herpes virus 8 (HHV-8) associated Castleman disease (strongly linked to mulicentric disease) [11,14]. Cases with mixed histologic features [5] and transition between the two types have been described [4].
1- Hyaline vascular:
The hyaline vascular sub-type accounts for 90% of cases of Castleman's disease [11] and patients are generally asymptomatic (58% to 97% of patients are asymptomatic). The median age at diagnosis is in the 3rd or 4th decade [11]. About 70% of affected patients are less than 30 years old, and males are affected more than females (females greater than males [4:1] in the AFIP series [7]), while other authors state that there is no sex preference [6,14]. Most patients are asymptomatic and come to clinical attention when a solitary middle or posterior mediastinal mass (adenopathy) is detected incidentally on chest radiographs [14]. Symptomatic patients may complain of dry cough, dyspnea, or recurrent infection due to airway compression. The disease is unicentric in 90% of cases [11]. In order of frequency, the intrathoracic sites involved include the anterior mediastinum, particularly right paratracheal, hilar nodes, and the posterior mediastinum. Lesions may demonstrate slow growth. Histologically, there is extensive capillary proliferation within the affected lymph nodes, and a lymphocyte predominant infiltrate surrounding small germinal centers. The treatment is surgical with a low recurrence rate if the resection is subtotal. Rare cases have been complicated by the development of vascular neoplasms that resemble Kaposi's sarcoma, or Hodgkins lymphoma [5]. Patients are also at risk for development of follicular dendritic cell neoplasms including dendritic cell sarcomas and stromal neoplasms [11].Treatment for unicentric disease is complete surgical resection [14]. With complete excision, the prognosis is excellent and the disease rarely recurs [14]. If surgical resection is incomplete, or the patient is a poor surgical candidate, XRT is a secondary treatment option [14].
2- Plasma cell variant:
Plasma cell Castleman represents less than 10% of cases [11]. In this form there is typically more generalized (thoracic, mesenteric, and retroperitoneal) lymph node involvement (although localized nodal involvement can be seen) and the disorder tends to be multicentric (although focal disease can be found in 10% (9-24% [11]) of cases). Histologically there are sheets of mature plasma cells within interfollicular tissues that surround normal to large germinal centers and the intense capillary proliferation seen in the hyaline vascular sub-type is absent. Dysregulation of interleukin-6 has been implicated in the pathogenesis of plasma cell Castlemans disease [7].An association with Kaposi's sarcoma associated herpes virus/ human herpes virus 8 (KSHV/HHV-8) has also been described [10]. Affected patients typically have systemic symptoms such as fever, weight loss, moderate anemia, elevated ESR, polyclonal hypergammaglobulinemia, and hypoalbuminemia. Patients with multicentric disease tend to be older individuals in their 5th or 6th decade. Treatment combines steroids and chemotherapeutic agents- although no single regimen has been effective in achieving a durable remission [5]. Prognosis is poor with an overall mortality of 50% and a median survival of 26 months [5]. Patients with multicentric disease and an associated neuropathy have an extremely poor prognosis despite treatment with steroids and chemotherapy. The clinical and histopathologic abnormalities associated with multicentric plasma cell variant Castleman's disease are similar to those found in osteosclerotic myeloma and the POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, monoclonal protein abnormality, and skin abnormalities) and some authors suggest an association between the two disorders (up to 37% of patients with multicentric Castlemans have POEMS syndrome and 11-30% of patients with POEMS syndrome have multicentric Castleman disease- most commonly the HHV-8 positive variant) [11]. As many as 50% of cases of POEMS syndrome coincide with sclerotic myeloma (however, only 1-8% of multiple myeloma patients have the sclerotic form) [11]. POEMS has a male predilection with a peak in the 5th-6th decades [11].
Patients with systemic Castleman disease (multicentric variant) are at increased risk for developing Kaposi sarcoma, follicular dendritic cell tumors, and Non-Hodgkins lymphoma (in up to 25% of cases- predominantly immunoblastic or plasmablastic B-cell subtypes) [11]. In patients with both HIV infection and multicentric disease the incidence of lymphoma is 15 fold higher than in patients with HIV infection alone [14].
Rituximab is the first-line teatment of multicentric disease in patients that are HIV or HHV8 positive [14]. Rituximab therapy has been shown to lead to improved survival and an 11 fold reduction in the development of lymphoma, especially in those with coexistent HIV infection [14]. In non-HIV and non-HHV8 patients, treatment options are less well defined [14]. Siltuximab, an antibody against endogenous IL-6, has been approved for therapy [14]. In patients with POEMS syndrome and multicentric disease, treatment usualy invovles high-dose immuno-suppressive agents and steroids [14]. If this fails, autologous peripheral blood stem cell transplantation is recommended [14].
3- HHV-8 associated Castleman disease:
HHV-8, also known as Kaposi sarcoma-associated herpes virus, is associated with multicentric Castlemans disease in HIV patients [11,13]. This represents the plasmablastic variant of Castlemans and is associated with a poor prognosis [11]. The disorder occurs predominantly in immunosuppressed and HIV patients (CD4 count <350 [12]), but the disease does not correlate with the CD4 cell count or the use of highly active antiretroviral therapy [11]. Other authors suggest the condition is more common in patients with a CD4 count above 200 cells/uL [13]. It manifests with generalized adenopathy, constitutional symptoms (fever, malaise, and weight loss [13]), and hematologic/immunologic abnormalities [11]. Treatment includes systemic chemotherapy and administration of anti-CD20 monoclonal antibody therapy [11]. Sustained remissions following anti-CD20 antibody therapy have been reported [11]. HHV-8 associated Castleman is associated with various lymphomas- specifically the HHV-8-positive plasmablastic large B-cell lymphoma [11]. Additional associations include Kapsoi sarcoma (most cases of HHV-8 associated Castleman disease coexist with KS [15]), primary effusion lymphoma, and hemophagocytic syndrome [11]. In HIV patients, the differential for avidly enhancing lymph nodes includes bacillary angiomatosis [12].
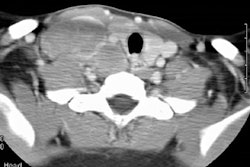
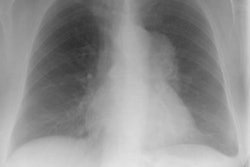
X-ray:
Localized form (Predominantly hyline vascular subtype): Plain film typically reveals a sharply marginated mass with smooth or lobulated borders within the mediastinum or hila [7].CT: Unicentric thoracic Castleman's can appear as a solitary non-invasive 5-7 cm mass (50% of cases), a dominant mass with involvement of contiguous structures (40% of cases), or matted lymphadenopathy confined to a single mediastinal compartment (10%) [9,11,14]. On unenhanced CT, the masses are typically homogeneous, but they can also appear heterogeneous. Following contrast administration there is generally marked homogeneous contrast enhancement of the mass (the plasma cell variant may not enhance to the same degree) [11]. Lesions have a tendency to lie on one side of the midline or over the hilum. The lesion may have poorly defined margins and invade contiguous structures [7]. Calcification is uncommon (5-10%)- typically punctate, coarse, discrete, central [4,7] or with a characteristic "arborizing" branching pattern [9,11].
MR imaging has been performed in a small number of cases and typically demonstrates heterogeneous signal intensity higher than skeletal muscle on T1 images and marked hyperintensity on T2 images [7]. Peripheral foci of decreased signal correspond to vascular flow voids [7]. The lesions enhance after the administration of gadolinium [7]. If diffusion-weighted imaging is performed, the mass will show restricted diffusion, with increasing signal intensity as the b value is increased [14].
On angiography, the masses in the hyaline vascular subtype show a prolonged dense tumor blush in the capillary phase. Pre-operative embolization has been used to decrease intra-operative bleeding [5].
Mulicentric variant (Predominantly plasma cell type):
There is typically no dominant mass. Multiple, moderate to avid
enhancing nodes may be seen in the chest, axilla, retroperitoneum,
mesentery, and inguinal regions (although in some cases only mild
enhancement is seen [14]). Splenomegaly and ascites may also be
seen in these cases [7].
Thin section CT findings include the presence of poorly defined
centrilobular nodules (due to an associated LIP [11]), thin-walled
cysts, and interlobular septal thickening [8]. These findings are
felt to be related to an associated lymphocytic interstitial
pneumonitis [8].
PET: Unicentric disease demonstrates moderate increased uptake on
FDG PET imaging [14].
REFERENCES:
(1) AJR 1996; Castleman's disease of the lung: radiographic, high-resolution CT, and pathologic findings.167: 1055-56 (No abstract available)
(2) J Thorac Imag 1997; Multicentric Castleman's disease and POEMS syndrome: CT findings.12: 75-77 (No abstract available)
(3) Curr Probl Diagn Radiol 1996; May/June 25(3):78-106
(4) Chest 1994; 105 (5) 1608-1610
(5) Mayo Clin Proc 1995; 70 (10): 969-977 (Subject review)
(6) Surgery 1992; 112(5): 850-855 (Subject review)
(7) Radiology 1998; McAdams HP, et al. Castleman disease of the thorax: Radiologic features with clinical and histopathologic correlation. 209: 221-228
(8) Radiology 1998; Johkoh T, et al. Intrathoracic multicentric Castleman's disease: CT findings in 12 patients. 209: 477-481
(9) AJR 2004; Ko SF, et al. Imaging spectrum of Castleman's disease. 182: 769-775
(10) AJR 2011; Davison JM, et al. FDG PET/CT in patients with
HIV. 197: 284-294
(11) Radiographics 2011; Bonekamp D, et al. Castleman disease:
the great mimic. 31: 1793-1807
(12) AJR 2012; Lichtenberger JP, et al. What a differetial a
virus makes: a practical approach to thoracic imaging findings in
the context of HIV infection- Part 2, extrapulmonary pulmonary
findings, chronic lung disease, and immune reconstitution
syndrome. 198: 1305-1312
(13) Radiographics 2014; Chou SHS, et al. Thoracic diseases
associated with HIV infection in the era of anti-retroviral
therapy: clinical and imaging findings. 34: 895-911
(14) Radiographics 2016; Kligerman SJ, et al. Castleman disease
of the thorax: clinical, radiologic, and pathologic correlation.
36: 1309-1332
(15) AJR 2021; Glushko T, et al. HIV lymphadenopathy: differential diagnosis and important imaging features. 216: 526-533