CHICAGO - What do referring physicians think of the radiology reports they receive, and how do they use them? Radiologists at Hershey Medical Center in Hershey, PA, conducted a survey to find out whether the reports they prepared met the needs of clinicians who received them.
A 16-question survey was designed to glean referring physicians' preferences of radiology report format, to determine how physicians read and extracted information contained in the report, and to find out how unexpected findings were handled. The survey was sent by internal e-mail to 607 staff physicians in March 2009. Data were collected using SurveyMonkey.com (Menlo Park, CA).
Dr. Rafel Tappouni, assistant professor of radiology in Hershey's abdominal imaging division, told RSNA session attendees that the lack of a standardized format for radiology reports and the wide variation in report quality, length, and format motivated him to initiate the project.
"When we issue a report, it is seldom that we get feedback regarding the quality of the report from the referring clinicians," he said. "The radiologist is unaware of how clinicians read the report and how often they interpret the images. In addition, it would be useful to know what clinicians' preferences are regarding communicating the report content to them and to their patients."
The radiologists received a 20% response to the survey, with the majority of physician respondents being internists, emergency department physicians, general family practitioners, pediatricians, and surgeons, as well as physicians representing 10 other specialties.
Findings
More than 90% of the respondents said they were comfortable interpreting x-rays -- 55.3% all of the time and 35.8% some of the time. More than half said they were equally competent at interpreting CT exams, with 31.4% for any CT exam and 37.2% for selective exams only. More than 60% left other types of modality exam interpretations (angiography, MRI, nuclear medicine, and ultrasound) strictly to radiologists, and 90% relied on radiologists to interpret mammograms.
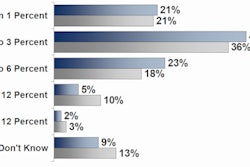
Depending on the type of exam, between 60% and 73% of the respondents read the entire radiology report that they received. Between 10% and 19% reported that they read the impression and part of the report.
About half of the respondents felt that report impressions contained useful findings 80% to 100% of the time. Between 5% and 10% reported that the impression section was not useful in up to 20% of the reports they received.
The majority of respondents, approximately 80%, requested that impressions be provided in numbered or bulleted format and that a standardized format be used. Only 19% liked the use of narratives or paragraphs to report impressions.
Referring physicians also requested that incidental findings be included in the impressions section of the report, even if they were benign. About half (51.3%) preferred that radiologists send an e-mail to notify them of a nonurgent critical results finding, and 27.4% preferred to be telephoned. The remainder felt that the radiology report provided ample notification, and the majority of respondents preferred radiologists to communicate exam findings to patients, especially when the patients asked the radiology department for the results.
Tappouni said that he and his colleagues were quite interested in learning if referring physicians wanted radiologists to talk directly with patients about the results of their diagnostic procedures. He reported that approximately 20% were adamantly opposed, 30% believed that this was an obligation of the radiologist, and approximately 50% had no objection if the patient initiated the request.
More than two-thirds of the respondents (67%) felt that it was appropriate for patients to receive a copy of their CT or MRI report directly from the radiology department to promote a patient's active involvement in their care. The survey did not include the question as to whether they should also receive a nondiagnostic quality DICOM CD of the exam that they could independently retain for their records.
Respondents were allowed to make multiple responses with respect to who is responsible for following up significant findings. Ninety-seven percent felt that it was the ordering physician's responsibility, but 65% of these same respondents stated that it was both the radiologist's and the patient's responsibility, and the responses were quite interesting.
With regard to follow-up of incidental findings that are significant and require further investigation, 14.2% supported the idea of mailing the radiology report to the patient, 40.6% supported the idea of designating an independent "office" to follow-up with patients, and 45% felt it was the responsibility of the patient's physician to contact them by phone or letter.
The survey also provided respondents with the opportunity to comment about improvements they would like to see the department make. Many focused on the need for the interpreting radiologist to make a commitment about the findings and not use language that hedged or avoided the reason the report was ordered. Either rule out something or don't, but don't put clinicians in the position of trying to interpret the radiologist's interpretation, was a primary complaint.
Physicians did not appreciate blanket recommendations, or use of the phrase "recommend ... if clinically indicated." They wanted the report to use medical terminology common to general practice, and for the department to eliminate variability in terminology.
Finally, they did not appreciate reading nonsense created by the speech recognition system that went undetected in the radiologists' report review and sign-off process.
Survey impact and follow-up
The radiology department held a workshop for residents in July 2009 as a result of the survey findings, Tappouni told AuntMinnie.com in a related interview. The objectives of the workshop were to improve the clarity of reports being generated, and to use the event to launch a department-wide initiative standardizing the basic format and style of radiology reports.
The workshop emphasized the use of simple, direct, and clear sentence structure and the elimination of uncommon abbreviations. Residents were reminded of the need to try and organize content by priority in the report, so that the highest priority findings are mentioned first, and also to number and list impression items in order of clinical importance.
"The main goal of this exercise was to improve the clarity and effectiveness of the report as a communication tool; however, the introduction of the new format standardization was also felt to be an important part of that process," Tappouni said.
The report format, which was implemented in August 2009, is simple and includes categories for exam title, clinical history, technique, comparison exams, findings, and impression.
"We have not adopted a true 'structured report,' per se, but rather merely a standardization of the basic paragraph style, so that all reports from our department have a similar outward appearance and the information in the report is organized in more or less the same way across all sections of our department," he explained.
Tappouni said that ongoing efforts will be made to ensure that standardization is consistent across all subspecialties and that everyone in the department is in compliance with the new report format.
The radiologists believe that by conducting a radiology report preparation workshop for residents, and by adopting the new report format and style, the quality of the radiology reports issued by radiologists will improve, according to Tappouni. However, he acknowledged that some of his colleagues had mixed feelings about making radiology reports too standardized.
The resident workshop will be an annual event, and a second survey will be conducted in 2010 to assess the Hershey clinicians' responses and to compare the findings of the 2009 and 2010 surveys.
Additionally, the residents were surveyed before and after the workshop to assess their impressions on whether the teaching intervention had the desired impact. A panel of physicians also will compare the residents' report clarity in random samples taken before and after the workshop to determine whether the workshop had a significant positive effect.
As a result of the survey, the radiology department is having discussions with Hershey Medical Center's risk management department and emergency department to explore the feasibility of delivering final radiology reports to patients before they leave the emergency department. Another option being considered is to mail copies of the report to the patient, with a cover letter for them to take on their next physician's visit. Whether these suggestions will be implemented has not yet been determined, Tappouni said.
By Cynthia E. Keen
AuntMinnie.com staff writer
December 3, 2009
Related Reading
Free library of best-practice report templates published by RSNA, December 2, 2009
It's hard to agree on what makes a good radiology report, November 12, 2009
Radiology reporting terms can confuse pediatricians, April 3, 2009
Format no factor in report efficiency, September 8, 2005
Radiology reports prone to language variability, June 3, 2005
Copyright © 2009 AuntMinnie.com