Physicians are more likely to view portal images via an electronic medical record (EMR) rather than on x-ray films, potentially leading to better care for patients receiving radiation therapy, according to a study in the July issue of the Journal of the American College of Radiology.
In fact, the authors of the study suggest that portal image review using an EMR should become a standard of care. If the study findings were followed by all cancer treatment centers, improper documentation issues related to portal image review could be reduced to nearly zero.
Portal images are used to verify patient positioning during daily radiation treatments to improve the accuracy of radiation field placement, to reduce exposure to normal tissue, and to deliver accurate dose to tumor volumes.
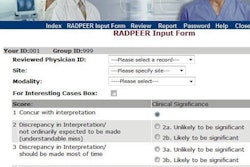
Researchers at Wayne State University School of Medicine and Barbara Ann Karmanos Cancer Center in Detroit conducted an analysis to determine whether electronic access to patients' portal images would affect the reporting behavior of the attending physicians who were reviewing them. The study was prompted by the facility's conversion in March 2010 to a version of its oncology information system (Mosaiq 1.60V4, Elekta) that supported portal image review via the EMR (JACR, July 2012, Vol. 9:7, pp. 495-497).
The researchers randomly selected 204 x-ray films of 22 patients who had portal images taken when treated between April 2009 and December 2009. Similarly, 207 digital portal images of 16 patients were randomly selected between April 2010 and June 2012. All of the patients had four or more portal images taken that were read by one of six attending physicians.
The policy of the radiation oncology department required that portal images be reviewed within one business day. Attending physicians were responsible for signing portal images for all of their patients treated throughout the day, with a rotating physician assigned to review any images that hadn't been reviewed at the end of the clinic day. Department policy also mandated that the date the portal image was performed be noted, and that attending physicians sign and date images.
When only x-ray films were available, the percentage of policy violations by the six attending physicians averaged 25% and ranged from 16% to 40%, according to lead author Dr. George Chen, a radiation oncology resident, and colleagues. One contributing factor may have been that there were no safeguards to prevent physicians from overlooking misplaced portal images. Another issue could be the inconvenience of having to physically go to the department to view portal images on x-ray films.
The severity of the violations were evenly divided: One-third of the images were not reviewed at all, one-third were not dated for either when they were performed or when they were reviewed, and one-third were reviewed after one business day.
Providing electronic access to review images dramatically reduced violations, Chen and colleagues found. The physician with a 40% violation rate had zero violations when using the EMR. Three other physicians also had flawless reporting records, and two physicians had a 2% violation rate, down from 25% and 17%.
"The use of an EMR for reviewing portal images dramatically improves compliance with timeliness and record keeping," said co-author Dr. Andre Konski, professor and chair of Wayne State's department of radiation oncology. "More timely review of portal images is critical because it allows for higher quality care in the treatment of patients with radiation."
Untimely review could lead to substandard treatments. The authors suggested that this was another reason for hospitals to invest in electronic patient records.
"Given this study's findings, in accordance with a nationwide push for transitioning to EMRs, reviewing portal images via an EMR should be a standard of care," they wrote.