The use of intensity-modulated radiation therapy (IMRT) for prostate cancer caused fewer toxicities and less cancer recurrence than conformal radiotherapy and proton therapy treatments, according to a study published in the April 18 issue of the Journal of the American Medical Association.
The study was part of special JAMA issue dedicated to comparative effectiveness research. Its findings were presented at an American Medical Association press conference held today at the National Press Club in Washington, DC.
More than 200,000 men in the U.S. are diagnosed annually with prostate cancer, and approximately 30,000 die each year from the disease. Treatment costs have been skyrocketing with the use of new approaches such as minimally invasive radical prostatectomy and new radiation therapy technologies such as IMRT and proton therapy (JAMA, April 18, 2012, Vol. 307:15, pp. 1611-1620).
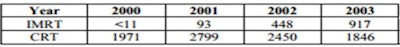
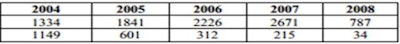
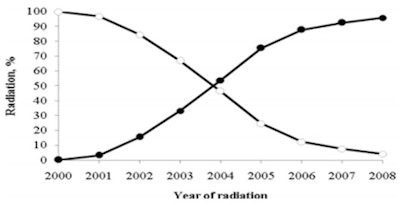
The type of radiation therapy used to treat prostate cancer has changed radically during the past decade. In 2002, more than 99% of men who were prescribed radiation therapy had conformal radiation therapy treatments. During 2004, this decreased to approximately 50%, and it decreased to 4% in 2008. By comparison, the use of IMRT increased from 0.15% in 2000 to 95.9% in 2008. Proton therapy began to be used in 2002, but its high cost of treatment and the scarcity of proton therapy centers severely limited its adoption, a situation that still exists today.
 |
|
|
|
|
| Use of IMRT vs. conformal radiation therapy (CRT) for primary radiation treatment for localized prostate cancer. Black circles = IMRT; white circles = CRT. Image courtesy of Dr. Ronald Chen, reprinted with permission of JAMA. |
The long-term effectiveness of various treatments for prostate cancer is not well-documented. The Institute of Medicine, the U.S. Agency for Healthcare Research and Quality, and the U.S. Department of Health and Human Services have been calling for comparative effectiveness studies, and the University of North Carolina in Chapel Hill responded to the request, said Dr. Ronald Chen, assistant professor of radiation oncology, at the media briefing.
Chen and colleagues used the Surveillance, Epidemiology, and End Results (SEER) Medicare-linked database to conduct a cancer recurrence outcomes and toxicities comparison. They identified 12,976 men who had been diagnosed with localized prostate cancer: 6,666 were treated with IMRT and 6,310 with conformal radiation therapy between 2002 and 2006. The authors identified 684 men treated with proton therapy between 2002 and 2007 and matched these patients with 684 who had received IMRT.
The median follow-up was 64 months for patients who had received conformal radiotherapy, 44 months for IMRT, and 50 months for proton therapy (with the IMRT-matched group followed for 45 months). Sophisticated analytic tools, including propensity score analysis, were used to produce the most comparable comparative results, Chen said.
The primary outcomes measured by Chen and colleagues were rates of gastrointestinal adverse effects such as rectal bleeding or diarrhea, urinary adverse effects, erectile dysfunction, and hip fractures. If additional cancer treatment was administered nine months or longer following treatment, the researchers categorized this as a cancer recurrence.
"We found that in the propensity score-adjusted analysis, men treated with IMRT were 9% less likely to experience gastrointestinal adverse effects and about 20% less likely to have a hip fracture than men treated with conformal radiotherapy," Chen said. "However, they had a slightly higher risk of erectile dysfunction."
Disease-free recurrence outcomes were also better for IMRT patients, with 2.5 patients per 100 patient-years requiring additional treatment, compared with 3.1 patients for conformal radiotherapy.
In the propensity score-matched comparison between IMRT and proton therapy, IMRT patients had a 34% lower risk of gastrointestinal adverse effects. However, the researchers did not find any other differences, which might have been influenced by the small sample size, Chen noted.
"Proton therapy is a high-profile, high-cost prostate cancer treatment," the authors wrote. "Since 2007, multiple proton facilities have been built, and direct-to-consumer advertising is likely to lead to a substantial increase in use. Overall, our results do not clearly demonstrate a clinical benefit to support the recent increase in proton therapy for prostate cancer."
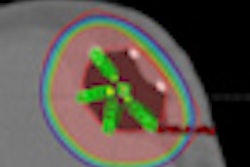
Chen attributed the nearly universal adoption of IMRT to its theoretical benefit of being able to target cancerous tumors better. This enables a higher radiation dose to be used and healthy surrounding tissues and organs to be increasingly spared. "Doctors want to offer the most effective treatments for their patients," he said.
Neither the published study nor Chen discussed the comparative costs of treatment. He said that this was outside the scope of the research, but he welcomed the "stitching together" of more outcomes studies, effectiveness studies, and cost-comparison studies.
Massachusetts General Hospital in Boston was conducting a randomized trial comparing the outcomes of prostate cancer patients treated with either IMRT or proton therapy, he noted. This could help answer the question of whether increasingly sophisticated radiotherapy is worth the increased cost, he said.