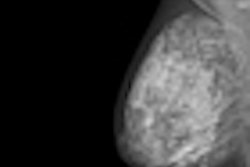
Women who receive at least three screening mammograms have a 49% lower risk of dying from breast cancer, according to a new study released online today in the journal Cancer Epidemiology, Biomarkers & Prevention, a publication of the American Association for Cancer Research (AACR).
Researchers at Erasmus Medical Center in Rotterdam, the Netherlands, used individual data for women invited to screening to conduct a case-control study to evaluate the effectiveness of population-based mammography screening in the Netherlands (Cancer Epidemiol Biomarkers Prev, December 6, 2011).
"Because the efficacy of mammography screening has been shown in randomized, controlled trials, the focus has turned on its effectiveness within daily practice," wrote lead author Suzie Otto, PhD, and colleagues. "[Ours] is the first case-control study that accurately accounts for equal screening opportunity for both cases and matched controls by number of invitations before case's diagnosis."
The Netherlands' national screening program was implemented gradually from 1989 to 1997 for women ages 50 to 69 years; in 1998, the upper age limit was extended to 75 years, Otto's team wrote. The program's recall rate is between 1% and 2%.
"Correcting for the gradual implementation [of the program], we showed that the downward trend in breast cancer mortality rates in the Netherlands was directly related to the initiation of the screening program," Otto's team wrote.
Otto and colleagues identified 755 patients who died from breast cancer between 1995 and 2003 and matched them with 3,739 controls. For each patient, the team had date of birth, date of screening invitations, date of screening examinations, screening status coded by attendance or nonparticipation, and the date of death, if applicable. The study also included data from the Comprehensive Cancer Center Rotterdam on breast cancer diagnosis; tumor stage according to the tumor, node, metastasis (TNM) classification of malignant tumors; and primary treatment, as well as causes of death data from a Statistics Netherlands database.
Mortality reduction
The researchers found that if women attended at least three screenings prior to diagnosis, their risk for mortality from breast cancer was reduced by 49%. The greatest reduction was seen in women between 70 and 75 years old, for whom the reduction in mortality was 84%. Among younger women (ages 50 to 69 years), the reduction was smaller, at 39%, but still statistically significant, the team reported.
Among the breast cancer cases, 29.8% were detected at screening, 34.3% were detected between screenings, and 35.9% of cases had never been screened.
What's more, fewer women who participated in screening had advanced cancers. Stage IV tumors were present in 29.5% of the never-screened cases but in only 5.3% of the screen-detected cases (stage IV tumors were found in 15.1% of the interval-detected cases).
"[Our findings show] that ... longstanding mammography screening in the Netherlands is effective in reducing the risk of breast cancer death," Otto and colleagues wrote. "[And these findings are] consistent with the outcomes of recent case-control studies of organized population-based mammography screening programs in Europe and Australia, with different performance indicators than seen in the Dutch program."
The case-control design for cancer screening has raised skepticism about its ability to evaluate the impact of screening activities, according to Otto's team, because it requires sophisticated selection procedures to identify all eligible cases within a source population. This is so that cases and matched controls are chosen according to eligibility criteria that ensure equal access to screening during the exposure period, and so that screening and diagnostic workup are distinguished from each other.
"The major strength of our study is that it was designed to correct for [these] drawbacks," the authors wrote.
Could the study findings be applicable in the U.S.? Perhaps, but the U.S. lacks a centrally organized government-funded program similar to what is found in the Netherlands, Otto said in a statement released by the AACR.
"The Dutch government considers it imperative that everyone eligible for a screening program is given the opportunity to participate," Otto said. "For that reason, all women in the targeted age group are invited and given the opportunity to decide independently to participate or not in screening programs that are entirely free of charge."
The study is yet another round in the ongoing duel between mammography backers and detractors regarding the effectiveness of population-based breast screening. An October study in the Archives of Internal Medicine estimated that mammography's mortality benefit could be as low as 5% to 10%, while Norwegian researchers in a paper presented at the American Society of Clinical Oncology (ASCO) Breast Cancer Symposium in September denied that breast screening had any mortality benefit at all.
Does the new study's relatively small sample size raise questions about the validity of the data, when compared to some of the larger population-based studies that have been published? Not at all, said Dr. Stephen Duffy of Queen Mary, University of London.
"This is a case-control evaluation, with a respectable number of cases," he told AuntMinnie.com. "I would have no concerns about the sample size. It is consistent with the prospective study results and suggests the Dutch screening program is doing a good job."