A series of editorials in this month's Journal of the American College of Cardiology examines radiation risk from cardiac imaging exams, and asks if the benefits of imaging have been understated in the risk-benefit equation to the detriment of patient care.
Better risk-benefit analyses and guidelines need to be developed and implemented, diagnostic exams that do not use radiation need to be carefully compared to current methods, and, probably most important, more money and effort will be needed to research these issues adequately, the authors concluded.
Exposing the public to ever-increasing amounts of radiation in the past several years has created fertile ground for a mismatch in the risk-benefit ratio that remains underrepresented in the literature, wrote Leslee Shaw, Ph.D., from Emory University School of Medicine in Atlanta, and colleagues in a summary of the articles.
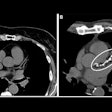
"The debate on the 'danger' of medical imaging has come to the forefront as a result of the rapid growth and wide-scale application of procedures exposing large segments of the U.S. population to ionizing radiation," they wrote. "For a cardiac imaging procedure, a focus solely on the risk of induced cancer can lead to imbalanced decision-making and disregard for the incremental detection of cardiac risk from procedures such as CT, SPECT, or PET" (JACC Cardiovascular Imaging, 2010, Vol. 3:5, pp. 550-552).
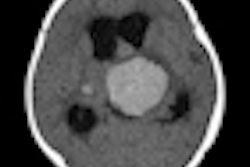
In one of the articles, Dr. Thomas Gerber, Ph.D., and Dr. Raymond Gibbons from the Mayo Clinic in Jacksonville, FL, cited National Council on Radiation Protection and Measurements (NCRP) data showing a 72% increase in per-capita radiation delivered to U.S. citizens from 1980 to 2006, primarily as a result of a 5.7-fold increase in dose from medical imaging. The rise in exposure is due largely to high-dose imaging exams including CT (49% of total radiation exposure) and nuclear medicine (26% of total exposure) (JACC Cardiovasc Imaging, 2010, Vol. 3:5, pp. 528-535).
The data show that a total of 3.1 million cardiac CT studies were conducted in the U.S. in 2006, representing 12.1% of the collective radiation dose to U.S. citizens, the authors noted. Even more frequent were the 18.1 million nuclear medicine studies in 2006, for which cardiac studies represented 57% of nuclear medicine visits and 85% of the collective radiation dose from nuclear medicine studies.
But risk is hard to assess
Unfortunately, radiation risk assessments are impossible to evaluate with any certainty, as they rely on the linear no-threshold (LNT) model derived from observation of atomic bomb survivors in Japan over decades, Gerber and Gibbons stated. The LNT model forms the basis of the most current radiation risk assessment, the Biological Effects of Ionizing Radiation (BEIR) VII report.
The LNT model assumes that the relationship between the relative risk of cancer and effective dose estimates extends linearly and without any threshold to patient populations, they wrote. But while LNT is considered the best-fitting model to weigh radiation dose against the lifetime attributable risk (LAR) of cancer, many experts caution against quantitatively estimating health risks at low doses. And because the LNT model is based on population-wide risk, it cannot be calculated at the level of the individual patient.
"Determining individualized, patient-specific estimates of radiation dose (and risk) is very complex, rarely done, and imperfect," the team wrote.
The likelihood of chromosomal changes that could lead to cancer increases with "cell proliferation, the number of future divisions, and the degree of differentiation of the cells in question," according to the authors.
Younger patients are considered to be at greater risk of cancer because their cells are more sensitive to radiation (as a result of a greater number of future cell divisions) than those of older patients. Older patients also get a reprieve for having lived through the latency period of 10 to 40 years for most radiation-induced solid cancers. And women are considered at greater risk due to the radiosensitivity of their breasts and lungs.
Therefore, the lifetime attributable risk of radiation exposure based on the LNT model from a single high-dose cardiac CT exam (21 mSv) is pegged at 0.7% (one in 143) for a 20-year-old woman, "nearly 16 times greater than that of 0.044% (one in 2,273) for an 80-year-old man," they wrote.
Still, cancer incidence doesn't reliably follow the LNT model, trending far lower than its predictions. In studies of radiation workers, standardized mortality rates are lower than those in the general population, a finding attributed to the "healthy worker effect."
"These potential risks of low-dose radiation must be weighed against the benefits of cardiac imaging," Gerber and Gibbons wrote. "Conceivable benefits of cardiac imaging include correct diagnosis, accurate prognostication, and improvement of patient outcomes. Such outcomes could include appropriate refocus on alternative noncardiac diagnoses (e.g., in patients with chest pain and normal SPECT studies), improved quality of life (e.g., attributable to relief of chest pain), and improved survival."
High- versus low-risk patients
Those patients at high risk of death and disability naturally have the greatest potential absolute gain from appropriate diagnosis and management, a risk that "varies with age, cardiovascular risk factors, symptoms, and previous evidence of coronary artery disease," they wrote.
On the other hand, "the benefits of imaging asymptomatic patients are more speculative, and compel that a higher bar be set for the use of radiation. The observed versus expected event rates across the range of predicted risk for models with and without imaging, the number of subjects reclassified across risk thresholds with the use of imaging, and the event rates of these subjects are not well established," the team explained.
They noted that the American Heart Association (AHA) has decided that calcium scoring may be considered in intermediate-risk patients, but not high- or low-risk patients. Nor are SPECT and coronary CT angiography recommended. New clinical practice guidelines from the AHA and the American College of Cardiology Foundation regarding the detection of asymptomatic coronary disease are scheduled for publication in 2010.
Gerber and Gibbons wrote that factors to consider in weighing the risks and benefits of healthcare include:
- Missing the right diagnosis in symptomatic patients by avoiding imaging
- Improved quality of life due to optimized therapy is difficult to quantify
- Improved survival due to optimal therapy versus possible decrease in survival from radiation-induced cancer
- Benefit-risk ratio is greater in symptomatic patients, high-risk patients, older individuals, and men
- Current evidence does not support imaging with ionizing radiation in asymptomatic individuals
- Benefit-risk ratio is improving as technical developments facilitate low-dose imaging with high image quality
In the absence of any proven benefit, the small projected increase in cancer risk "argues against the widespread use of SPECT or CT angiography in asymptomatic individuals but even more so does their cost," Gerber and Gibbons stated.
Practically speaking, patients who undergo cardiac imaging are often older and more likely to die of illnesses including cardiac disease than from radiation-induced cancer.
"Unfortunately, this important concept is often lost in the controversy surrounding asymptomatic individuals among healthcare professionals and the media coverage of radiation risk in the lay press," they wrote.
The Centers for Medicare and Medicaid Services (CMS) is planning a pilot study of imaging appropriateness, the team noted.
"Appropriately choosing the right test for the right patient and performing it with the lowest possible radiation dose to the patient remains a challenge, both to those who order imaging studies and those who perform them," they wrote.
Sensible steps
In another article, Sandra Halliburton, Ph.D., and Dr. Paul Schoenhagen from the Cleveland Clinic Foundation advised an approach that emphasizes carefully assessing the risk-benefit ratio of every exam, along with significant additional work to improve and standardize the tools available to make the assessment.
"Efforts to date have primarily included the development of appropriateness criteria and the implementation of dose-lowering techniques," they wrote. "Still needed is the development of standards that incorporate radiation exposure optimization into scan protocol selection. Such standards must consider applied radiation in the context of the clinical indication, as well as the characteristics of the patient, and provide guidance with regard to specific parameter settings (JACC Cardiovasc Imaging, 2010, Vol. 3:5, pp. 537-540).
Well-designed quality standards must consider applied radiation in the context of the clinical indication, patient characteristics, the availability of alternative diagnostic strategies, and the specific CT imaging technique available.
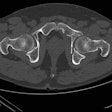
For some patients, such as a 30-year-old man with symptoms suggesting aortic dissection, the decision is straightforward. Avoiding the radiation dose associated with CT would be inappropriate, but the patient could be followed up using cardiac MRI, Halliburton and Schoenhagen noted.
On the other hand, determining what to do with a female patient in her 40s with atypical chest pain inquiring about a cardiac CT would be more difficult.
"While CT angiography may be appropriate for the clinical situation, the patient should be advised about alternative imaging and nonimaging diagnostic strategies, even if low-dose CT imaging is available," they wrote, emphasizing the need for a "comprehensive, individualized review of the clinical scenario" and the standards before cardiovascular CT is performed.
Clinical experience has enabled the development of guidelines for cardiovascular CT that weigh "procedural risk, pretest probability, and expected benefit," Halliburton and Schoenhagen wrote. A significant reduction in radiation dose for a particular indication "could shift the risk-benefit ratio and subsequently have an impact on appropriateness criteria. However, the relatively noninvasive nature of a test alone does not establish its usefulness for screening, in particular because false positives in patients with low pretest probability can be associated with untoward outcome."
Guidelines must be considered in the context of similar guidelines for other imaging tests. And if CT is considered the most appropriate test, the imaging protocol must be tailored to the clinical question, they wrote.
"For example, assessment of coronary anatomy requires high spatial resolution and, subsequently, high tube current to achieve acceptable image noise," they wrote. "In contrast, for the assessment of noncoronary cardiovascular anatomy (e.g., evaluation of pulmonary vein or aorta), lower spatial resolution may be sufficient, permitting the reconstruction of thicker slices and the lowering of x-ray tube current during data acquisition."
It won't be easy. The establishment of well-developed criteria has been hindered by the rapid development of scanner hardware and software and differences in scanner design, they said. And good research is expensive.
Large imaging centers handle imaging criteria by forming collaborative multimodality imaging groups that include "radiologists, cardiologists, physicists, and technologists," Halliburton and Schoenhagen noted.
The team's proposed initiatives include promoting patient awareness of medical radiation issues, "expanding appropriateness criteria into clinical decision-making, incorporating safeguards into scanner designs, developing radiation dose reference values for specific procedures, incorporating radiation dose values into the electronic medical record, creating a national dose registry, establishing minimum standards for training and education of imaging personnel, and expanding mandatory accreditation for advanced imaging facilities," they wrote.
While much has already been accomplished to establish standards and adhere to them, much more work will be required to ensure optimal patient care, Halliburton and Schoenhagen concluded.
For their part, Shaw and colleagues, who reviewed all of the articles in the JACC issue, envision a multifaceted approach to the future that creates high-quality evidence that can be clearly assimilated by patients and physicians.
"We need more guidance documents from cardiovascular specialty and imaging societies to synthesize current evidence and guide the effective use of cardiac imaging procedures that do or do not expose patients to ionizing radiation," they wrote. "The cardiac imaging community also needs to devise patient educational Web sites that fully inform the public on appropriate decision-making on the risks and benefits of cardiac imaging. For clinical research, mandatory inclusion of radiation safety as an end point would be an important goal and would further our understanding of radiation-induced risk."
In addition, cardiac imaging radiation "should become a strategic priority for funded research" that includes comparative effectiveness studies with modalities that use radiation versus those that do not.
According to Shaw and colleagues, effective test decision-making will also require:
- Reliable measurement methods
- A standard approach for extrapolating high- to low-dose exposure situations
- Methods for estimating radiation-induced risks in imaging cohorts with an elevated cancer risk
- Meaningful effective dose categories that are risk-based and relevant to cardiac imaging
In this vein, the American College of Radiology (ACR) has devised a radiation risk level that is integrated within the society's appropriateness criteria, focusing on minimizing patient radiation, they noted.
Among the questions to be answered are when radiation-free exams can be substituted for studies that deliver ionizing radiation, and the effects of cumulative exposure. The answers will require a considerable boost in research over past levels but will be well worth the cost.
"Given the sizeable population at risk for cardiovascular disease, such evidence would greatly contribute to reducing cardiac morbidity and mortality without disrupting projected national statistics for cancer incidence," Shaw and colleagues concluded.
By Eric Barnes
AuntMinnie.com staff writer
May 14, 2010
Related Reading
Young adults face higher CT radiation risk than seniors, May 4, 2010
Studies spotlight high CT radiation dose, increased cancer risk, December 14, 2009
NEJM study: Imaging procedures, radiation growing, August 26, 2009
Web site educates patients about radiation dose, July 2, 2009
BEIR VII and separating fact from fear, November 18, 2005
Copyright © 2010 AuntMinnie.com