Whole-brain CT perfusion with a volume helical shuttle (VHS) technique provides rapid confirmation of whether patients have suffered a stroke or transient ischemic attack (TIA), according to studies presented last week at the American Academy of Neurology (AAN) annual meeting in Toronto.
The new data also indicate that volume helical shuttle doesn't expose patients to more radiation than a previous version of volume shuttle CT, according to researchers from California Pacific Medical Center's Comprehensive Stroke Care Center in San Francisco.
VHS provides whole-brain CT perfusion coverage, starting at the top of the spinal column. California Pacific is currently the only U.S. facility using VHS with CT perfusion, which was implemented at the center in November 2009 on a scanner developed by GE Healthcare of Chalfont St. Giles, U.K. The technology comprises some software along with minor hardware modifications to standard CT equipment.
Dr. Nobl Barazangi, Ph.D., and colleagues confirmed the utility of volume helical shuttle CT perfusion by reviewing the records of the 102 patients evaluated with the technique at the center through January 2010 for possible stroke or TIA.
The center's protocol involves acquiring VHS CT perfusion sections, with postprocessing reconstruction to 2.5-mm thickness. The software also allows production of thinner or thicker slices. The scans took an average of 11 minutes to complete.
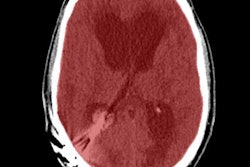
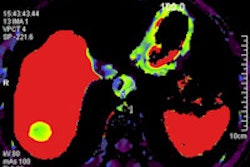
The workups confirmed that 33 of the patients had a stroke and another 27 had a TIA. CT perfusion mismatch -- that is, increased relative mean transit time (rMTT) but symmetrical regional cerebral blood volume (rCBV) -- was found in 36% of the stroke and 19% of the TIA patients; this is indicative of ischemic penumbra. In addition, 27% of the stroke patients had matched CT perfusion defects, which are represented by increased rMTT and reduced rCBV, and which point to a completed infarct.
Of the stroke and TIA subjects, 21 in each group also underwent an MRI within 24 to 48 hours of admission. The results correlated in 67% of the stroke cases and 100% of the TIA cases. In the remaining seven patients, small lacunar infarcts of multifocal small embolic infarcts were seen on MRI.
|
|||||||||||||||
| *rt-PA = recombinant tissue plasminogen activator |
The investigators also compared 2.5-mm and 5-mm VHS CT perfusion images in several patients. This confirmed that the thinner slices can detect infarcts that may be invisible with 5-mm sections.
"We've found VHS CT perfusion is useful in cases where it is not clear whether the patient has suffered a stroke," Barazangi, a physician in stroke, neurocritical care, and neurology, told AuntMinnie.com. "It can also help with neurointerventional treatment decisions."
In a companion study led by Dr. Jack Rose, the team tallied the patient radiation exposure from optimized VHS CT perfusion to that from volume shuttle (VS) CT perfusion, an earlier version of the volume shuttle technology. They found that VHS produced slightly lower radiation dose than VS.
The investigators identified 36 consecutive patients who underwent comprehensive stroke CT imaging with VS and a further 17 consecutive patients who underwent VHS CT perfusion.
The mean total dose-length product (DLP) was 7,253 ± 424 mGy-cm with VS CT perfusion and 6,127 ± 591 mGy-cm with VHS CT perfusion. Moreover, the respective average effective doses were 16.7 ± 1.0 mSv and 14.1 ± 1.3 mSv.
The team noted that these levels are within safety guidelines produced by the U.S. Food and Drug Administration (FDA). They also are comparable to the 6,790 ± 722 mGy-cm DLP and 16.4 ± 2.4 mSv means reported in a cohort of patients who underwent comprehensive stroke CT imaging with more limited CT perfusion coverage (Neuroradiology, October 2009, Vol. 51:10, pp. 635-640).
"We now do VHS on all of our patients with suspected stroke, or with subarachnoid hemorrhage with vasospasm," Rose said. He added that they are vigilant not to overimage the latter group of patients, who are younger than the former patients.
By Rosemary Frei
AuntMinnie.com contributing writer
April 20, 2010
Related Reading
Resting fMRI exam may predict stroke and brain injury outcomes, March 30, 2010
MRI links silent stroke to kidney failure in diabetics, February 1, 2010
Stroke assessment varies depending on CT perfusion software, January 22, 2010
Clinical exam more predictive than postsurgical head CT, December 21, 2009
Ultrasound signals of asymptomatic emboli predict stroke risk, December 7, 2009
Copyright © 2010 AuntMinnie.com