A new brain tumor imaging technique based on optical coherence tomography (OTC) may offers surgeons a highly accurate way to visualize -- and ultimately resect -- malignant tumors during surgery, according to a report from Johns Hopkins University.
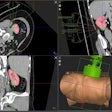
The technology could give surgeons a color-coded map of the patient's brain that clearly delineates the areas that do not have cancer, enabling the removal of cancerous tissue with great accuracy, wrote lead author Dr. Carmen Kut, PhD, and colleagues in Science Translational Medicine (June 17, 2015, Vol. 7:292).
The technique can potentially be used for intraoperative guidance and to provide direct visual clues in real-time, said co-author Xingde Li, PhD, a professor of biomedical engineering at the university, who developed the tool in his bioengineering lab.
"The technique itself is noninvasive, and it operates in real-time in a noncontact fashion," Li told AuntMinnie.com.
Quantitative differences
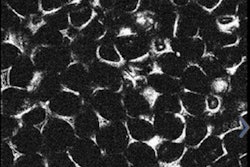
Brain surgery is complicated by the need to remove as much tumor tissue as possible without resecting healthy tissue, when it is often difficult to distinguish the two visually, according to the authors. Quantitatively, however, there are differences between brain tumor and healthy tissue, and OCT can readily distinguish them.
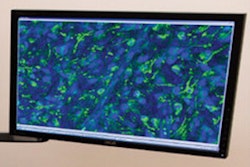
The tumor "is invisible or at least very subtle to the naked eye," Li said. But it fairly jumps out of the screen in OCT when seen under infrared light, making it possible to quantify the image's optical properties over the volume being imaged. Optical properties can then be color-coded, making it easier for surgeons to visualize areas of interest.
After all, color is what you see of it, according to Li. The brain's white matter appears white because "when you look at it in sunlight or under a bright light, the tissue basically bounces all the color back," he said.
If you look at brain tissue under OCT, you see light reflecting from the myelin sheath covering healthy tissue. However, in regions with cancer, the myelin sheath is degraded -- offering a reliable marker that a computer algorithm can use to distinguish the two tissue types.
"Visually, the difference between the two tissue types is very subtle, but quantitatively the change is easy to see in optical attenuation," Li said.
Also, because the light that shines on the tissue is near-infrared, operating in direct room light will not change the color-coded brain image seen on the monitor. To determine the location of cancerous tissue, the group uses a visible aiming beam that functions as a kind of a laser pointer in bright green.
As a result, the surgeon knows at every moment "where he is aiming, or cutting, with the green spot," Li said.
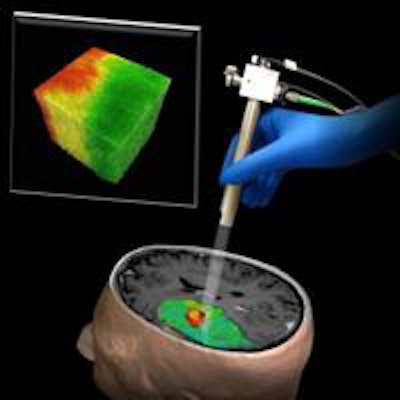
Once the study team determined how healthy and cancerous brain tissue could be distinguished by density and even more easily by color, they built the algorithm to process the OCT data and almost instantaneously generate a color-coded map. In the map, tumor appears in red and healthy tissue in green, giving the surgeon a continuously updated picture on a monitor of the exact tissue locations.
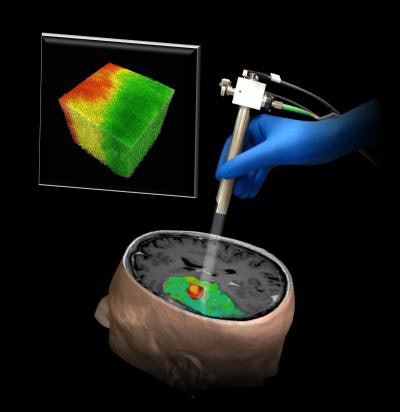 The new OCT technique could help surgeons distinguish tumor (red) from surrounding noncancerous tissue (green). Image courtesy of Dr. Carmen Kut, PhD; Dr. Jordina Rincon-Torroella; Xingde Li, PhD; Dr. Alfredo Quiñones-Hinojosa; and John Hopkins Medicine.
The new OCT technique could help surgeons distinguish tumor (red) from surrounding noncancerous tissue (green). Image courtesy of Dr. Carmen Kut, PhD; Dr. Jordina Rincon-Torroella; Xingde Li, PhD; Dr. Alfredo Quiñones-Hinojosa; and John Hopkins Medicine."We think optical coherence tomography has strong potential for helping surgeons know exactly where to cut," said co-author Dr. Alfredo Quiñones-Hinojosa in a statement.
On to humans
To date, the technique has worked quite well in experiments that used fresh brain tissue removed from mice. The goal is to begin clinical trials as soon as possible, with a pilot study beginning perhaps as soon as the fall, according to Li.
If studies confirm the utility of the technique, clinicians will have access to an intraoperative image-guidance modality that is substantially better than conventional modalities, he said. For example, ultrasound suffers from low resolution, and MRI is expensive and slow.
In addition, MRI "doesn't offer continuous intraoperative guidance," Li said. "You move patients into the magnet, you do imaging for 30 to 50 minutes, and then you pull the patient out of the magnet."
In contrast, the OCT system is fast and high-resolution, and it can be built for around $100,000, he said. The research is being funded by the U.S. National Cancer Institute (NCI), the National Institute of Biomedical Imaging and Bioengineering (NIBIB), and the Coulter Foundation. The group is also evaluating the technique for other cancers and applications, such as blood vessel visualization, where OCT might offer a breakthrough.