PET/MR images have led researchers for the first time to confirm evidence of neuroinflammation in key regions of the brain in patients with chronic back pain, according to a study published online January 12 in Brain.
A group from Boston detected elevated levels of a translocator protein that is associated with neuroinflammation and is a marker of glial cell activity. By demonstrating glial activation in chronic pain, the findings suggest that glial cells could eventually be used as a therapeutic target and to help develop biomarkers for pain conditions.
Previous studies have found a link between glial activation and persistent pain in animal models, but no research had documented glial activation in the brain in humans with chronic pain.
"Until very recently, we thought chronic pain conditions arose from dysfunctioning neurons within the pain path networks or the central nervous system," said lead author Marco Loggia, PhD, an assistant professor of radiology at Harvard Medical School and assistant professor of neuroscience at Massachusetts General Hospital (MGH). "But in the past 10 years or so, there has been a 'revolution' in pain research, as it was discovered in animals that glial cells within the central nervous system and the brain have a very important role in the establishment of pain."
Novel radiopharmaceutical
Loggia and colleagues also had the benefit of using a carbon-11-labeled radioligand (C-11 PBR28) recently developed by the National Institutes of Health (NIH). The agent is designed to bind to the translocator protein and visualize glial activity and neuroinflammation.
"We now have the opportunity to use this ligand that binds in vivo to activated glia," Loggia told AuntMinnie.com. "We were able to test the hypothesis, and it turns out that it looks like it's true that a patient with chronic back pain exhibits activity of glia in the brain."
The researchers enrolled 19 patients who had chronic lower back pain for at least two years (age range, 29 to 63 years) and 25 healthy control subjects (age range, 28 to 65 years). From that cohort, they paired 10 chronic lower back pain patients with nine pain-free control individuals based on gender, age, and genetic characteristics (Brain, January 12, 2015)
Imaging was performed on a 3-tesla MRI scanner (Magnetom Tim Trio, Siemens Healthcare) equipped with an eight-channel head coil and a dedicated PET insert designed for brain imaging (BrainPET, Siemens) and simultaneous PET/MRI acquisition. The subjects intravenously received a median dose of 11.2 mCi of C-11 PBR28.
"The main advantage to using PET/MRI in this particular study is that we could collect structural images of the brain, which were used for anatomical reference and for attenuation correction," Loggia said. "This is beneficial for the patients because it reduced the amount of time spent lying in the scanner and discomfort for patients with chronic back pain."
There is also less radiation exposure to a patient with the use of MRI for attenuation correction, rather than using CT for the same purpose.
Glial revelations
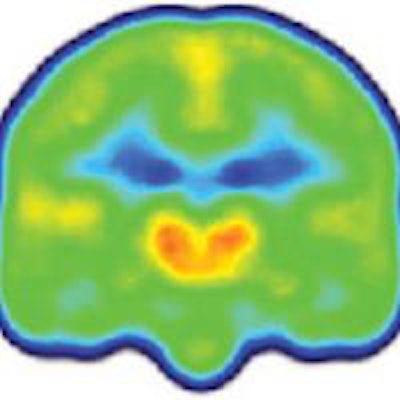
PET/MRI revealed glial activation through C-11 PBR28 binding and significantly higher levels of the translocator protein in the thalamus and other brain regions in patients with chronic lower back pain versus the control subjects.
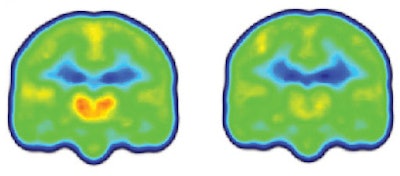 Images created by averaging PET scan data from chronic pain patients (left) and healthy controls (right) reveal higher levels of inflammation-associated translocator protein (orange/red) in the thalamus and other brain regions of chronic pain patients. Images courtesy of Marco Loggia, PhD.
Images created by averaging PET scan data from chronic pain patients (left) and healthy controls (right) reveal higher levels of inflammation-associated translocator protein (orange/red) in the thalamus and other brain regions of chronic pain patients. Images courtesy of Marco Loggia, PhD.The distinction was so consistent across the subjects that the researchers could differentiate between the two groups simply by looking at the individual images, before a statistical analysis was performed.
Loggia and colleagues also found that patients who reported lower levels of pain had the highest levels of the translocator protein. Animal studies have suggested that the protein may actually limit the extent of the glial response after it is triggered, which could explain the finding, according to the group.
The researchers chose this patient population for the study because chronic back pain is such a prevalent condition. However, Loggia surmised that the PET/MRI technique to detect glial cell activity could be used with other chronic pain ailments.
He and fellow researchers at the MGH-based Martinos Center for Biomedical Imaging are using PET/MRI with the C-11 PBR28 radioligand to image inflammation across a number of conditions.
"One of the questions is: Is it possible to identify potential glial signatures with, for example, a fibromyalgia patient, who may have a pattern of glial activation that differentiates it from chronic back pain?" he added.
The researchers also recently published a paper on using the ligand for patients with amyotrophic lateral sclerosis (ALS).
"All of this work is important for two reasons," Loggia said. "First, it provides a rationale for exploring glial modulation as a therapeutic approach in these patients, rather than using other pain drugs," he added. "There also is no real biomarker now to know whether you are in pain and how much pain. The possibility of measuring glial activation may be a step forward in the certification of the biomarker for pain."