Despite its ability to improve the detection of breast cancer, breast MRI computer-aided detection (CAD) software still misses some. Several factors can affect the detection capabilities of the software, Korean researchers have found.
In a study involving more than 300 breast cancer patients, a team from Kangbuk Samsung Hospital discovered that histopathology factors such as tumor type, invasiveness, and low nuclear grade were associated with the cancer detection performance of breast MRI CAD. A low Ki-67 percentage was the only significant immunochemistry factor.
In light of these findings, radiologists should check immunohistologic profiles and the original images when interpreting breast MRI CAD results, according to a team led by Dr. Seon Hyeong Choi. Choi presented the results during a scientific session at RSNA 2013 in Chicago.
Breast MRI CAD performance
CAD systems for breast MRI provide pixel-by-pixel kinetic information of dynamic enhancement above a certain threshold level. While it's been known to improve specificity for breast cancer by better demonstrating the presence of enhancement and delayed-enhancement features, CAD still doesn't detect some cancer cases, Choi said.
Breast cancer is often divided into subtypes based on the expression of immunohistochemical (IHC) markers, and these IHC factors affect the treatment plan and, most importantly, patient outcomes.
As a result, the researchers sought to evaluate the histopathological and IHC factors affecting breast MRI CAD's performance for detecting breast cancer. They retrospectively reviewed 356 breast cancer patients who underwent MRI between July 2011 and February 2013.
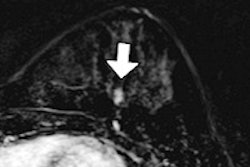
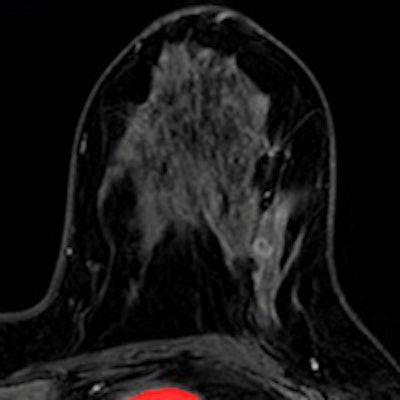
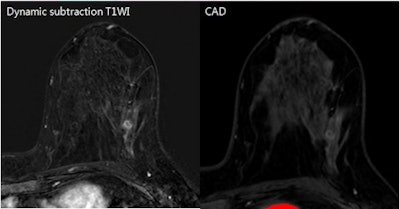 False-negative breast MRI CAD result in patient with an approximately 1-cm metaplastic carcinoma in her left breast. Contrast-enhanced subtraction image (left) shows an irregular rim-enhancing mass, suggesting a typical malignant-looking mass. MRI CAD results (right) did not show a color map, however. The patient had a low Ki-67 percentage. Images courtesy of Dr. Seon Hyeong Choi.
False-negative breast MRI CAD result in patient with an approximately 1-cm metaplastic carcinoma in her left breast. Contrast-enhanced subtraction image (left) shows an irregular rim-enhancing mass, suggesting a typical malignant-looking mass. MRI CAD results (right) did not show a color map, however. The patient had a low Ki-67 percentage. Images courtesy of Dr. Seon Hyeong Choi.After 32 cases were excluded due to conditions such as no residual cancer after excision or chemotherapy, no operation after excision, no IHC results, and carcinomas of unknown primary origin, the remaining 324 patients with 327 histologically proven breast cancers were included in the study.
In patients with multifocal or multicentric cancers, only the index cancer was analyzed. The researchers also analyzed each breast in cases of bilateral cancer.
Preoperative breast MRI was performed on an Achieva 3-tesla scanner (Philips Healthcare) and included unenhanced T1- and T2-weighted turbo spin-echo (TSE) axial images, dynamic contrast-enhanced images (one precontrast and five postcontrast axial images, as well as a fat-suppressed T1-weighted 3D fast-field echo sequence), and a postcontrast axial T1 sequence for workup of axillary lymph nodes. 3D maximum intensity projection (MIP) reconstruction was also performed.
The researchers applied CADstream breast MRI CAD software (Merge Healthcare) using a 50% threshold of initial enhancement. They then retrospectively reviewed the CAD results and noted the patient's age, histopathological factors (such as lesion size, pathological size, invasiveness, nuclear grade, and the presence of extensive intraductal components), and IHC factors.
CAD detected 259 (79.2%) of 327 cancers but missed 68 (20.8%). The mean patient age in the group with undetected cancers was 50 ± 9.9 years, compared with 51.4 ± 10.7 years for detected cancers. The mean tumor size in the group undetected by CAD was 18 mm (range, 1-70 mm), compared with 22.8 mm (range, 3-120 mm) for the detected cancers.
| Breast MRI CAD performance | ||
| Undetected by CAD | Detected by CAD | |
| Pathology | ||
| Invasive ductal carcinoma (n = 242) | 32 (13.2%) | 210 (86.8%) |
| Ductal carcinoma in situ (n = 57) | 26 (45.6%) | 31 (54.4%) |
| Invasive lobular carcinoma (n = 13) | 5 (38.5%) | 8 (61.5%) |
| Others (n = 15) | 5 (33.3%) | 10 (66.7%) |
| Cancer invasiveness | ||
| Invasive (n = 269) | 41 (15.2%) | 228 (84.8%) |
| Intraductal (n = 58) | 27 (46.6%) | 31 (53.4%) |
| Lesion nuclear grade | ||
| 1 (n = 35) | 14 (40%) | 21 (60%) |
| 2 (n = 189) | 39 (20.6%) | 150 (79.4%) |
| 3 (n = 82) | 13 (15.9%) | 69 (84.1%) |
| Presence of extensive intraductal component | ||
| Negative | 56 (21.5%) | 204 (78.5%) |
| Positive | 9 (22.5%) | 31 (77.5%) |
"[The study findings] suggested that you can miss many [ductal carcinoma in situ (DCIS)] if you don't check the original images on PACS," Choi told AuntMinnie.com.
Tumor type and invasiveness significantly affected CAD detection performance, while a nuclear grade of 1 was negatively correlated. Looking at IHC factors, only a low Ki-67 percentage (0-14%) was significantly associated with CAD performance (present in 26.3% of missed cancers).
Although the breast MRI CAD software showed good performance, it did not detect about 20% of breast cancers, the researchers concluded.
"Histopathology of tumor type and invasiveness were significant factors affecting breast MRI CAD [detection performance]," Choi said. "Low nuclear grade -- grade 1 -- was negatively correlated with detection rate. Immunohistochemistry factors were not significant except for Ki-67."