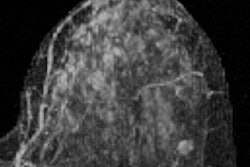
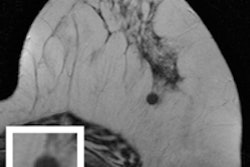
Conventional x-ray mammography is a notoriously poor tool for screening women with dense breast tissue. Breast MRI is a possible alternative, but the cost of the exams is prohibitively high. A Michigan breast specialist believes he has changed the equation with a streamlined breast MRI screening exam that could be ready for widespread clinical use.
But wait, it gets better: Breast specialists using the streamlined breast MRI exam in the state will even get paid for it starting November 18. That's when HealthPlus of Michigan will begin paying for annual breast MRI screening exams in addition to mammography for women who have at least 50% fibroglandular tissue based on volume.
 Dr. David Strahle of Regional Medical Imaging.
Dr. David Strahle of Regional Medical Imaging.The exam is based on a protocol developed by Dr. David Strahle, president of Regional Medical Imaging in Flint, MI. He believes that MRI is the gold standard for finding breast cancer, but it hasn't been accepted on a routine basis because of cost and high biopsy rates. His protocol addresses both concerns.
"Clinical literature says that mammography eventually finds 85% of breast cancers, but for women with dense tissue, it's often too late by the time the cancer is detected," Strahle told AuntMinnie.com. "MRI is near 100% sensitive for finding cancer in dense breast tissue. It's the exam we've been waiting for, and it's been available all along."
More cancers found
In a study conducted between June 2009 and June 2011, Strahle and colleagues invited 671 women who had a negative or benign screening mammogram to undergo a free breast MRI exam. Women with recent positive mammograms or a personal history of breast cancer or those who were BRCA-positive or who had contraindications to MRI were not included in the study.
For each woman, Strahle's team recorded data for 18 parameters, including percent volume and density of any fibroglandular tissue, as well as the location of any lesions inside or outside fibroglandular tissue.
The researchers found that using several streamlined MRI sequences that Strahle developed for women with 50% or more fibroglandular tissue identified an additional six cancers missed by mammography in the patient population. This would translate into 16.3 additional cancers detected per 1,000 women per year.
In the general population, mammograms detect 2.7 cancers per 1,000 women per year, according to Strahle. At this rate, "it would take [mammography] six years to identify all 16.3 cancers seen on breast MR," he told AuntMinnie.com. "So for women with dense tissue, breast MR shifts time of detection up to six years earlier than screening the same patients with mammograms."
Strahle's group reduced the cost of the exam to $395, less than half of a typical MRI. It's not much more than the average cost of screening mammography, he said.
"When you include additional views, ultrasound, occasional MRIs, or biopsies, the average screening cost for mammography is about $252 in Michigan," he said. "The difference between these two is only $143, and this difference is only in women with dense breast tissue."
In the study, Strahle's team also cut the unnecessary biopsy rate, from mammography's eight unnecessary biopsies per 10 procedures performed to four out of 10.
Further work
Strahle's original work was intended to identify a usable screening breast MRI protocol for replacing and/or augmenting annual screening mammography. But his team has continued to conduct research to evaluate how a national breast MRI screening program might save lives and reduce costs.
"We've been evaluating how standardized techniques for interpretation of the images by radiologists could be developed, how MR technologists could be trained in the proper use of the protocols, and how the protocols would work on the five most common MR scanners in the U.S.," Strahle told AuntMinnie.com.
To this end, in September of last year, the group began screening with MR using Strahle's protocol in women with dense breasts who were willing to pay the $395 fee themselves. He and his colleagues also created a presentation geared toward payors that outlines the financial advantages of an annual breast MRI screening program for women with dense breast tissue.
"We went to insurance companies and showed that the protocol not only would save women's lives, but that the financial savings would be so substantial that insurers could pay for both mammography and screening breast MRI and still yield a significant net savings," he said.
Their work paid off. HealthPlus of Michigan announced it will begin paying for annual screening breast MRI studies for its female members who have at least 50% fibroglandular tissue. Four other insurance companies have expressed interest in covering the protocol as well, Strahle said.
The company plans to start with its commercial HMO patients between the ages of 40 and 80, according to board chairman Miles Owens.
"Our goal is to detect breast cancer early and save lives, and we're convinced that this MRI breast imaging protocol can do that," Owens told AuntMinnie.com.
Michigan lawmakers have also taken notice. On October 17, Strahle will present information about the new protocol at a forum for Michigan's Legislature hosted by state Rep. Winnie Brinks (D-Grand Rapids). Brinks has proposed HB 4260, which would require women with dense breast tissue to be notified of their status and that other more-advanced technologies besides mammography are available to further address the problem.
A 2-tiered approach
One potential drawback of using only MRI for screening women with dense breasts is that some early cancers are identified by calcifications alone on mammograms, and breast MRI might initially miss these. Therefore, Strahle and colleagues are proposing a two-tiered approach to the early detection of breast cancer: They would screen women who have at least 50% fibroglandular tissue by volume by augmenting mammograms with breast MR, then convert to screening with mammography only for less than 50% tissue density.
This kind of approach could begin now, without breast centers necessarily having to buy any new screening technology, according to Strahle.
"Mammography is a 50-year-old technology, and it's just not effective in women with dense tissue," he said. "We need to find these cancers early, and we can do that with screening breast MRI."