A group of California breast imagers and breast cancer risk specialists has launched a website to help radiologists and referring physicians navigate the challenges posed by breast density notification laws, according to a report published online September 10 in Radiology.
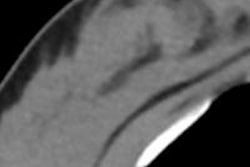
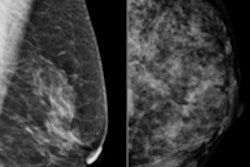
Mammography is still considered the best modality for population-based breast cancer screening. But its sensitivity decreases by up to 20% in women with dense breast tissue, the researchers wrote. In response to this problem, several states -- including California -- have passed legislation that mandates women be notified after mammography exams of their tissue density. Women should also be made aware of adjunct imaging modalities for breast cancer screening such as ultrasound and MRI, according to the legislation.
California's version of the law went into effect on April 1. Because approximately 50% of women who undergo screening mammography have breast tissue that is classified as heterogeneously dense or extremely dense -- and are therefore eligible for density notification letters -- that could mean 2 million letters sent per year in California alone, the researchers wrote.
Breast density notification boosts patient awareness, but there are downsides, including unsubstantiated patient anxiety, the potential for misunderstanding or overestimating risk, and an increased tendency to overscreen, according to report contributor Dr. Jafi Lipson from Stanford University School of Medicine (Radiology, September 10, 2013).
 Dr. Jafi Lipson from Stanford University School of Medicine.
Dr. Jafi Lipson from Stanford University School of Medicine."Given that very large numbers of women will be receiving breast density notification letters, it made sense to us to craft guidelines for referring physicians about how to handle further consult with their patients," Lipson told AuntMinnie.com. "The legislation is a reality, and we wanted to be proactive in responding to it from a practice perspective."
Lipson and colleagues from various University of California campuses formed the California Breast Density Information Group (CBDIG) in 2012. Over the next nine months, before the law's April implementation date, the group created an online document that addresses radiologist and referring physician questions about the efficacy, benefits, and harms of supplementary screening tests. The document also includes a PDF primer for healthcare providers, as well as one for patients about breast density from the American College of Radiology (ACR).
Why the need for this document? California law doesn't come with guidance for physicians about how to proceed after a woman has been notified of breast density, and its broad classification of density doesn't take into account the varying risk levels among patients with different breast densities, according to Lipson and colleagues.
"When risk is expressed relative to average breast density, the risk for the 40% of women with heterogeneously dense breasts is about 1.2 times greater than average, and the risk for the 10% of women with extremely dense breasts is about 2.1 times greater than average," the group wrote. "Therefore, breast density is a risk factor, but not a strong one."
Overall, CBDIG recommends an individualized, risk-based approach for guiding the decision-making process about whether women with dense tissue should have supplemental screening, Lipson said. Women with a high risk of breast cancer, such as those with the BRCA genetic mutation, are more likely to benefit from additional screening with MRI, ultrasound, or tomosynthesis; however, for women at intermediate risk, the decision to have additional screening should be made on a case-by-case basis, using a shared decision-making approach between the patient and her doctor.
"Supplemental screening recommendations should be based in the context of other breast cancer risk factors, not just on density," Lipson told AuntMinnie.com. "Rather than notification automatically triggering an additional test, we hope it will spark a discussion between women and their doctors about their overall breast cancer risk."