Lung cancer patients with invasive tumors near vital structures are often thought to be inoperable cases. But these patients could gain new hope thanks to a dynamic 4D wide-area CT technique that is able to see the tumors in motion, helping clinicians give the go-ahead for surgical resection.
In what an Australian group is calling the first use of differential motion to diagnose lung cancer in wide-area CT scanning, 10 lung cancer cases previously deemed inoperable were downstaged and resected after 4D CT (3D with motion) showed the tumor moving separately from adjacent structures. In nine of the 10 pilot cases using the technique, the more optimistic diagnosis turned out to be correct, and surgery was successful.
Residual tumor was left in just one of the patients, and the interpretation error of that scan could be seen retrospectively, according to lead author Dr. John Troupis, from Monash Medical Centre in Melbourne.
Preliminary results in eight patients were presented at the RSNA 2012 meeting, but the group has now analyzed the results of the 10 patients in preparation for peer-reviewed publication, Troupis said.
Hope for inoperable cases
A finding of invasive lung cancer at CT staging most often leads to the case being deemed inoperable. Without the ability to see a space between the tumor and the aorta or chest wall, it's impossible to tell if a mass is invasive, and that usually means no surgery, Troupis said in an interview with AuntMinnie.com.
"If it's invaded though the wall and it's attached firmly, the surgeon won't risk the patient's life" because the patient might still have a year or two to live without surgery, he said.
But Troupis and other Monash researchers developed a technique that employs wide-detector CT acquired during a continuous scan in which the patient continues to breathe. The breathing motion itself often reveals displacement of the tumor vis-à-vis the surrounding anatomy during respiration, changing the diagnosis, said Troupis, who heads the musculoskeletal imaging section and serves as co-unit head of cardiac at Monash Medical Centre's Cardiovascular Research Centre.
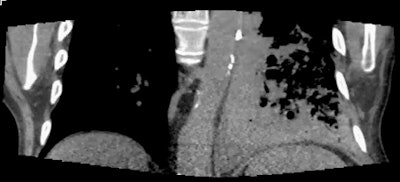
Forced expiration during imaging "moves the cancer away from the chest wall or away from the aorta, and everything moves at different rates," he said. Detection of differential motion between two adjacent nontethered structures suggests that the tumor can be surgically removed.
Troupis and colleagues including Sundeep Pasricha, Stephen Stuckey, Julian Smith, and Cliff Choong examined a new technique for utilizing the wide 16-cm z-axis coverage of a 320-detector-row CT scanner (Aquilion One, Toshiba Medical Systems), which provides high-resolution images using a nonspiral setting that scans continuously without table feed. High-resolution 4D images can be evaluated as a motion volume dataset in any plane. Routine staging CT scans were acquired first, and used to guide the field-of-view.
The scanner acquires six volumes per second at reasonable radiation doses that are edging downward with experience toward 5 mSv per case. Each image volume is acquired in about two to three seconds and contains a couple thousand images, Troupis said; a single case might comprise 10 volumes and 20,000 to 40,000 images.
The scanner's wide coverage area makes it possible to scan larger tumors than would be possible with a typical 64- or 128-detector-row machine, which would be limited to 4 cm or 8 cm of anatomy, Troupis said. The wide anatomic coverage is needed because otherwise "when the patient breathes, you're expecting [the tumor] to move more than 1 to 3 cm and you'd be out of the field-of-view," he said.
 |
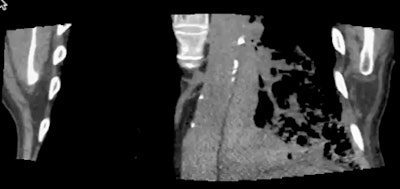 |
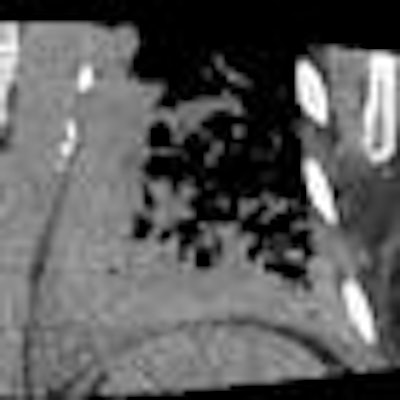
| In a patient with a left lower adenocarcinoma, conventional staging CT was unable to exclude invasion of the left lateral aspect of the aorta. However, static images (one at extreme inspiration and one at extreme expiration, above) and two coronal video files (below) confirm differential motion, and the tumor was confirmed at surgery. Images and cine clips courtesy of Dr. John Troupis. |
 |
 |
The latest data now include 10 patients (6 men; average age, 69.6 years) with lung cancers adjacent to vital structures or the chest wall. All had biopsy-proven carcinoma with poorly defined planes between the tumor and the adjacent structure, but without metastatic disease.
The patients were coached to perform a full respiratory cycle in 3.5 sec, and gantry rotation of the scanner was set to the minimum of 350 msec, Troupis said. The mA was based on the patient's body mass index (BMI), and intravenous contrast media was administered prior to scanning in four cases where a vascular structure was involved. Data were reconstructed in multiple image planes depending on tumor location. The radiologist and the thoracic surgeon interpreted the images in consensus.
Differential motion was evaluated qualitatively, though a quantitative assessment system using a 2D grid was developed later to improve assessment, Troupis said.
In six cases, the tumor was abutting the chest wall, including three cases in which the tumor was adjacent to major vessels, and three cases of tumors in the lung apex. Another patient had a 1.4-cm spiculated right upper-lobe mass and suspected pleural involvement, but 4D CT confirmed a lack of pleural tethering.
One patient with a large right upper-lobe mass adjacent to the superior vena cava was a false negative, as the tumor could not be completely resected at surgery, but the correct diagnosis could be seen retrospectively, Troupis said.
"Though all were true negatives with no invasion, one was difficult to remove off the major vein of the chest, and, in fact, residual disease was left on that vein, so [the tumor] wasn't completely removed," he said. Looking back at the CT images, "we could see where we went wrong, but we missed it," he said. "The imaging was correct; the problem was with us."
In a real-time workstation analysis, 4D CT imaging revealed differential motion between cancer and the adjacent structure in nine of the cases. Intraoperative assessment confirmed resectability of the cancers in nine of the 10 cases analyzed to date. Today, all patients remain alive one to five months after surgery.
But what about dose?
Radiation doses have come down as the group has gained experience, Troupis said. The dose for the first patient was 57 mSv, whereas the dose for the last patient was 4.2 mSv. The average dose for the 10 cases was 16.3 mSv; excluding two patients with elevated doses brought the average down to 11.9 mSv.
The potential of this technique for diagnosing more operable cancers is significant, Troupis said. His institution alone sees perhaps 10 to 15 new lung cancers every week, of which 5% to 15% -- or one to two cases -- may appear inoperable at conventional staging CT.
For Troupis, who has done a lot of work in 4D CT, including a paper on joint motion, 4D CT is extremely promising, and the heart is another area with potential for the technique.
"In the past, we've had a lot of patients [who] would not have been offered surgery," he said. "I don't have any concrete data about that, but I believe it's happened in the past and that it still happens today, and 4D CT could assist in further evaluation."