The use of Doppler ultrasound to monitor fetal health during high-risk pregnancies improves outcomes by decreasing the number of both cesarean sections and perinatal deaths, according to a new meta-analysis from the Cochrane Collaboration of London.
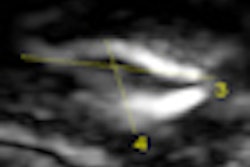
In a Cochrane systematic review of fetal and umbilical Doppler ultrasound in high-risk pregnancies, a research team led by Dr. Zarko Alfirevic of the University of Liverpool in the U.K. examined 18 studies with an aggregate of 10,000 women in high-risk groups. The reviewers concluded that Doppler ultrasound of the umbilical artery should be performed in high-risk pregnancies thought to be at risk of placental insufficiency, although the authors acknowledged shortcomings related to the current body of research.
"The quality of the current evidence was not of high quality, therefore, the results should be interpreted with some caution," the authors noted. "Studies of high quality with follow-up studies on neurological development are needed."
False-positive findings
Although the detection of abnormal fetal blood-flow patterns on Doppler ultrasound may indicate poor fetal prognosis, false-positive findings may also encourage inappropriate early delivery, according to the research team. In a review supported by a grant from the U.K. National Institute for Health Research, the study team sought to assess the effect on patient care and fetal outcomes of Doppler ultrasound used to assess fetal well-being in high-risk pregnancies (Cochrane Database of Systematic Reviews, 2010, Issue 1).
The authors searched the Cochrane Pregnancy and Childbirth Group's Trials Register and reference lists of identified studies. For inclusion in the review, studies had to be randomized and quasirandomized controlled trials studying use of Doppler ultrasound for investigating umbilical and fetal vessel waveforms in high-risk pregnancies.
Two authors independently assessed the studies for inclusion and bias risk; data extraction was then performed. Any disagreements were resolved by discussion or by involving a third author.
The 18 studies included research comparing the use of Doppler ultrasound with no Doppler ultrasound or with cardiotocography (electronic fetal monitoring). Research examining uteroplacental ultrasound was excluded, as that will be the subject of a future Cochrane review. However, studies were included if umbilical artery or fetal Doppler exams were combined with uteroplacental Doppler.
The authors considered two primary outcome measures:
- Any perinatal death after randomization
- Serious neonatal morbidity -- composite outcome including hypoxic ischemic encephalopathy, intraventricular hemorrhage (IVH), bronchopulmonary dysplasia (BPD), and necrotizing enterocolitis
Twenty-six secondary outcomes were also examined.
While the researchers found the trials to be generally of unclear quality with some evidence of possible publication bias, the use of Doppler ultrasound in high-risk pregnancy was associated with a statistically significant reduction in perinatal deaths (risk ratio = 0.71, 95% confidence interval: 0.52 to 0.98; data from 16 studies and 10,225 babies).
Doppler ultrasound also led to fewer labor inductions (average risk ratio = 0.89, 95% confidence interval: 0.80 to 0.99; data from 10 studies and 5,633 women) and fewer cesarean sections (risk ratio = 0.90, 95% confidence interval: 0.84 to 0.97; data from 14 studies and 7,918 women).
In other results, the authors did not find any difference in operative vaginal births (risk ratio = 0.95, 95% confidence interval: 0.80 to 1.14; data from four studies and 2,813 women) or in Apgar scores less than 7 at five minutes after birth (risk ratio = 0.92, 95% confidence interval: 0.69 to 1.24; data from seven studies and 6,321 babies).
While Doppler ultrasound studies of the umbilical artery should be performed in high-risk pregnancies thought to be at risk of placental insufficiency, the definition of suspected placental insufficiency, the frequency of Doppler studies, and delivery timing in the event of an abnormal Doppler study remain elusive variables, the researchers noted.
"Women with hypertensive disorders and small for date fetuses are obvious candidates whilst the role of umbilical artery Doppler in other risk groups like post-term, diabetes and uncomplicated dichorionic twin pregnancy is still debatable," the authors wrote.
The researchers did not recommend, however, the routine clinical use of more sophisticated Doppler tests such as blood-flow assessment in the middle cerebral artery and ductus venosus. These exams have not yet been rigorously evaluated in clinical trials, the authors wrote.
The authors believe a case could be made for a larger trial of Doppler ultrasound than has been performed to date, particularly in risk groups with a relatively low risk of fetal growth restriction caused by impaired placental blood flow.
"Observational studies suggest that fetal vessels other than the umbilical artery may be better markers of fetal well-being, fetal ductus venosus in particular," the authors noted. "It is hoped that future clinical studies evaluating possible added benefit of these tests will comply with the most recent CONSORT statement (www.consort-statement.org) and use clinical outcomes from this Cochrane review as the minimum dataset."
By Erik L. Ridley
AuntMinnie.com staff writer
January 20, 2010
Related Reading
Study finds sharp rise in prenatal ultrasound use in Canada, January 7, 2010
Screening for Down syndrome can start with biochemistry, November 12, 2009
Diagnosis, abortion of Down's babies rising in U.K., October 27, 2009
Ultrasound not needed for infants with single umbilical artery, July 16, 2009
Copyright © 2010 AuntMinnie.com