A couple of months ago I attended the grand opening of a ritzy department store in downtown San Francisco. The city's mayor, Gavin Newsom, was also at this shindig, glad-handing his way through a throng of admirers. In fact, people lined up in front of the store's perfume counter just for the privilege of shaking Mayor Newsom's hand.
But I declined to cue up and, as it turns out, I did the mayor a huge favor. Occupational therapists recently released a bulletin warning politicos against overuse injuries brought on by excessive hand-shaking.
Too much grip and grin can lead to pain and stiffness in the hands, arms, neck, and back, according to the pamphlet published by American Occupational Therapy Association. Politicians were advised to warm up with hand exercises before public appearances and ice down afterward.
Come November 8 (postelection day in the U.S.), if whistle-stoppers find themselves in need of medical attention for hand and wrist injuries, they'll be happy to know that imaging is bipartisan: Both MRI and ultrasound are equally valuable for assessing such conditions as tenosynovitis, skier's thumb, and vascular flow.
Throw your hands up in the air for MRI
Contrast-enhanced, 3D MRI angiography (MRA) of the hand has made serious inroads as an alternative to the more invasive imaging methods. But 3D MRA does pose its own challenges in the very small vessels of the hand.
"MR angiography ... is a new and promising method ... for evaluation of the peripheral arteries of the palmar arch," explained Dr. Thomas Gluecker and colleagues from University Hospital Basel in Switzerland. "However, various physiologic conditions must be considered. The most important is the short arteriovenous circulation time, which may cause early and significant venous contamination, thereby reducing data quality and diagnostic outcome" (American Journal of Roentgenology, October 2006, Vol. 187:4, pp. 905-910).
One possible explanation for this contamination is the venoarteriolar reflex, which consists of precapillary arteriolar vasoconstriction, the authors stated. Using cuff compression during hand MRA seems to regulate the venoarteriolar reflex, resulting in reduced arteriolar flow.
For this study, Gluecker's group enlisted 10 healthy subjects, all of whom underwent three MRA studies on a 1.5-tesla unit (Magnetom Sonata, Siemens Medical Solutions, Malvern, PA) over seven days. During each study, a different flow rate of venous injection was used: 0.5 mL/sec, 1.0 mL/sec, and 1.5 mL/sec.
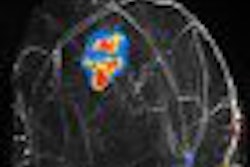
 |
| Maximum intensity projection from reconstructed 3D contrast-enhanced MR angiography of both hands of 25-year-old healthy male volunteer after IV administration of gadobutrol using a flow rate of 0.5 mL/sec. Imaging sequence was obtained 40 seconds after initiation of contrast injection. Subsystolic cuff compression is applied to upper arm on right side. Major venous contamination (venous contamination score = 2) is observed on noncompressed left side. Gluecker TM, Bongartz B, Ledermann HP, Bilecen D. "MR Angiography of the Hand with Subsystolic Cuff-Compression Optimization of Injection Parameters" (AJR 2006; 187:905-910). |
Upper arm compression was applied unilaterally with a standard blood pressure cuff during all three studies. "Subsystolic compression was performed with a pressure value of 30% less than the brachial artery systolic blood pressure measured by the examination," the authors explained. The volunteers received 0.1 mg/kg dose of gadobutrol followed by a saline flush for each 140-second-long study.
All 10 subjects completed the exams and tolerated the cuff compression, the authors stated in their results. For all three flow rates, a contrast-to-noise ratio (CNR) of more than 10 was obtained. In the venous vessels, the least venous contamination was measured with a flow rate of 0.5 mL/sec.
On qualitative analysis, this latter flow rate starting at 60 seconds was given the highest score by the reviewers. Conversely, studies performed with an injection rate of 1.5 mL/sec received the worst score for venous contamination.
Diminished venous contamination was seen on the compressed side for all flow rates, the group reported. Again on qualitative analysis, both reviews saw less venous contamination on the compressed side and with a flow rate of 0.5 mL/sec.
The authors acknowledged that their sample size was small and that the results may differ in patients with problematic hands, such as vasospasm, vascular stenosis, or trauma. Still, these results are promising, they noted. They also recommended that reducing the applied pressure to 50% less than the brachial artery systolic blood pressure for even better results.
In the second paper out of Switzerland, Dr. Marco Zanetti and colleagues shared their MR technique for assessing chronic wrist pain. In terms of equipment, optimal imaging can be achieved by using a dedicated wrist coil, sections of 2-3 mm, and a field-of-view of 8-10 cm, according to the group from University Hospital Balgrist in Zurich.
For the imaging protocol, they recommended an injection of gadolinium and iodinated contrast into the distal radioulnar joint (DRUJ) for direct MRA. For indirect MRA, they used a dose of 0.1 mmol/kg.
"Indirect (MRA) is based on the concept that contrast material injected intravenously, over time will diffuse into the joint space, so that quasiarthrographic T1-weighted imagines can be obtained," they wrote (European Radiology, August 24, 2006).
In terms of patient positioning, the authors stressed that "attention should be paid to avoid excessive radial and ulnar deviation as this will affect normal sagittal radiolunocapitate alignment."
Zanetti's group then offered some MR pearls and pitfalls in various areas of the wrist. These included the following:
Complete tears of the triangular fibrocartilage (TFC) complex are visualized better on MR than partial tears, with excellent results reported for central or radial TFC lesions. Both conventional arthrography and MRI may miss TFC ulnar attachment tears.
MR's sensitivity is generally higher in scapholunate ligament tears versus lunotriquetral ligament tears.
In tendinitis, thickening of the tendon and increased T1-weighted signal intensity can be seen. Partial tears lead to increased signal intensity on T2-weighted imaging as well. Thickened tends of the first compartment and synovial edema may be de Quervain's synovitis.
Gadolinium-enhanced MR is ideal for detecting avascularity of bone in patients with pseudoarthrosis. Occult bone lesions are seen as signal intensity abnormalities in the subchondral bone marrow.
1.5-tesla MR is inaccurate for detecting focal articular cartilage defects in the radiocarpal joint.
Several presentations at the 2006 RSNA in Chicago will focus on MRI in the hand and wrist. One education exhibit (LL-MK5272) will correlate MR findings in osteoarthritis of the hand with x-ray and anatomic signs. A scientific paper (SSJ22-01) will compare MR, CT, and MR arthrography in wrist ligament tears.
US: The whole world in its hands?
In work-related wrist tenosynovitis, ultrasound is best deployed as a second-line classification technique, according to occupational health specialists from Italy. Dr. Cristiana Fiorentini and colleagues looked at the potential epidemiological use for ultrasound in a population of 160 production workers.
"Tenosynovitis of the wrist frequently accompanies forceful and repetitive wrist-hand activities, especially when associated with awkward wrist posture," wrote Fiorentini, who is from the Policlinico Sant'Orsola-Malpighi in Bologna. "We analyzed data collected ... from a population of meat (processing) workers highly exposed to biomechanical risk factors" (Occupational and Environmental Medicine, September 14, 2006).
The workers were assessed by a biomechanics expert for hand activity level and peak finger force while on the job. An occupational physician examined the workers clinically for signs of wrist tenosynovitis and carpal tunnel syndrome.
Ultrasonography was done on a unit with a 7.5-MHz linear transducer. The tendons of the flexor digitorum muscle were examined at the palmar compartment of the wrist. The transducer was placed parallel and proximal to the distal crest in the transverse scan, and parallel to the palmaris longus tendon in the longitudinal scan, the authors explained.
"The following ultrasonography findings were recorded: 1) nonhomogeneity of tendinous bundle echotexture; 2) thickening of the tendinous bundle; 3) anechoic halo around at least one tendon," they added.
These sonographic parameters are commonly considered pathognomonic of acute and degenerative tendon pathology, the authors said. The anechoic halo around the tendon is considered a hallmark of synovitis.
According to the biomechanical analysis, the workers repeated 30 hand-related actions per minute. Clinical symptoms included tenosynovitis in 33% of the workers. On imaging, only 22% of the symptomatic workers showed any ultrasonographic signs, the authors reported. Also, each of the three sonographic findings showed good specificity at 85% or higher, but low sensitivity at less than 60%. Overall, the poor concordance between ultrasound findings and symptoms indicated that pain is not a specific enough symptom to define tenosynovitis.
This led the authors to suggest that ultrasound, when paired with symptom-based definitions of the disease, may overestimate the frequency of wrist tenosynovitis. However, they added that in symptomatic subject, sonographic information can produce more specific epidemiological classification.
"The better definition of small, superficial tendons provided by a 10-MHz linear probe could be more informative," they stated in their conclusion. "Furthermore, use of power Doppler technology to distinguish between hypoechoic fluid (serous tenosynovitis) and synovium (hypertrophic tenosynovitis) could provide another potentially relevant ultrasonography finding for future investigations."
Moving from the wrist to the thumb, radiologists from the U.S. and Belgium used ultrasound to diagnose ulnar collateral ligament (UCL) tears of the thumb.
"UCL injuries are common, and the management dilemma is whether to treat them conservatively or surgically," wrote a group led by Dr. Farhad Ebrahim from the University of Michigan Health System in Ann Arbor. Ebrahim's co-authors are from Aalsters Stedelijk Ziekenhuis in Aalst, Belgium, and the University of Liége in Liége, Belgium (RadioGraphics, July-August 2006, Vol. 26:4, pp. 1007-1020).
UCL tears, also called gamekeeper's thumb or skier's thumb, and damage are caused by hyperabduction of the metacarpophalangeal joint, exacerbated by varying degrees of hyperextension. Referring physicians, who sometimes have difficult examining UCL tears because of pain and swelling, will often request "stress radiographs," but these are difficult to interpret, Ebrahim's group stated.
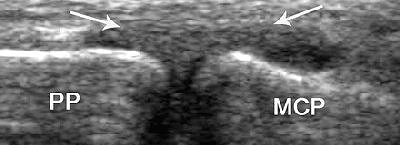 |
| UCL strain in a 32-year-old man. Coronal US scan of the thumb shows diffuse thickening of the UCL (arrows) without a tear. MCP = metacarpal, PP = proximal phalanx. |
"The spectrum of UCL injury includes strain, partial-thickness tear, and full-thickness tear. We outline a simple method of performing (ultrasound) of the thumb and discuss the spectrum of common acute disorders encountered with particular emphasis on UCL injuries," they wrote.
In their sample of 32 patients, ultrasonography was performed with the hand placed flat on a table. A 12- to 23-MHz linear probe was slid from the second finger onto the first metacarpophalangeal joint to obtain either a transverse image of the UCL or a longitudinal one.
In general, the UCL tear is considered displaced when it is retracted or folded on itself. It will also move proximal to the adductor aponeurosis, which creates the appearing of a yo-yo on a string, according to the authors. The yo-yo portion is the torn, displaced UCL.
Ebrahim's group offered a number of ways to use ultrasound to make the differential diagnosis between UCL injury and other conditions.
In ulnar side dorsal hood injury, dynamic ultrasound will illustrate the injured tendon and any dislocation to the ulnar when the thumb is flexed. When the tendon is trapped in the anatomic snuffbox, it can often be misdiagnosed as a UCL tear, they cautioned.
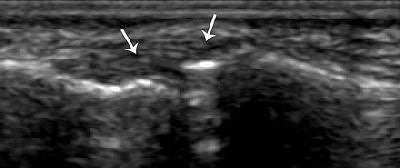
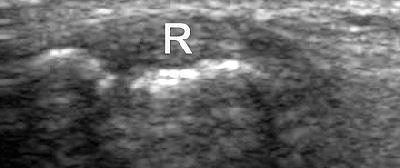 |
| Strain of the radial collateral ligament. The left side of the images is distal. Above, coronal US scan of the thumb shows a thickened elongated radial collateral ligament (R). Below, coronal US scan of the contralateral thumb, obtained for comparison, shows a normal radial collateral ligament (arrows). "US Diagnosis of UCL Tears of the Thumb and Stener Lesions: Technique, Pattern-based Approach, and Differential Diagnosis," Ebrahim FS, et al. RadioGraphics 2006;26:1007-1020. |
 |
In radial side ligament injury, look for distinctive patterns of instability, they stated. A disrupted UCL, along with dorsal capsular tears, is likely to result in combined radiovolar subluxation. Disruption of the radial collateral ligament is more likely to produce a rapid sequence of joint instability and, ultimately, degenerative disease.
For de Quervain's disease, ultrasound should demonstrate swelling of the affected tendons and a hypoechoic pattern with areas of heterogeneity. In palmar-side trigger thumb, the extended finger may become trapped and ultrasound allows for closer evaluation of tendon integrity.
Because UCL tears can be treated conservatively, the authors stressed the importance of looking for the degree of displacement on ultrasound.
For more on sonography of the wrist and hand, an RSNA education exhibit (LL-MK4840) will offer a comprehensive review for detecting lesions, tendon injuries, and foreign bodies. Also, a refresher course (RC804) will delve into the hand and wrist in sports imaging.
By Shalmali Pal
AuntMinnie.com staff writer
November 6, 2006
Related Reading
Low-field dedicated extremity MRI useful for assessing early rheumatoid arthritis, September 8, 2006
Part I: Choosing between MR and US in musculoskeletal imaging, September 7, 2006
Ultrasound allows precise tendinitis treatment, May 11, 2006
The twisted tale of skier’s thumb: A case study, September 15, 2002
Copyright © 2006 AuntMinnie.com