The use of on-board imaging (OBI) can improve the accuracy of intensity-modulated radiation therapy (IMRT) in the treatment of patients after surgery for prostate cancer by enabling oncologists to narrow their field of treatment, according to a new report by California researchers.
A group of researchers led by Dr. Ajay Sandhu from the University of California, San Diego (UCSD) in La Jolla used an OBI device to guide IMRT treatments in a group of prostate cancer patients. Their findings were published online June 4 in the journal Radiotherapy and Oncology.
The adoption of IMRT has been a major advance in radiation therapy by enabling oncologists to conform radiation dose to the shape of the target, sparing healthy tissue and resulting in lower toxicity to the patient. OBI takes radiation therapy to the next level by enabling the IMRT system to make adjustments in real-time based on data from an imaging device sitting alongside the treatment system. This can help correct for issues like patient motion during treatment.
In IMRT of the prostate, understanding prostate bed movement is critical for precise delivery of radiation therapy because IMRT employs tight margins around the target. Because such tight margins are used, significant dosimetric consequences can occur if even small errors arise from organ motion and patient setup.
The UCSD researchers wanted to see just how tightly they could narrow the margin between treatment fields and healthy tissue by using a commercially available OBI system. They studied the technique in 26 postprostatectomy patients receiving treatment at the UCSD Medical Center. OBI replaced electronic portal imaging devices, ultrasound-based systems, or weekly CT scans as the technique used to correct for setup error and organ motion.
OBI is likely to be more efficient and less time-consuming, with the least amount of interuser variability, when used for daily setup prior to each treatment, according to Sandhu, the medical director of the department of radiation oncology and principal investigator at UCSD for the Radiation Therapy Oncology Group (RTOG). Patients are also able to avoid the radiation dose from weekly CT scans.
Radiotherapy using OBI
The group treated 26 patients, ranging in age from 52-77 years (mean, 62 years), with adjuvant or salvage radiotherapy between September 2005 and March 2007 at the UCSD Medical Center. Patients with positive margins, seminal vesicle invasion, or extra-prostatic extension received adjuvant radiotherapy. Patients with rising prostate-specific antigen levels following radiation therapy received salvage radiotherapy.
All patients were treated with an image-guided radiation therapy (IGRT) technique aimed at the prostate bed and underwent treatment planning simulation in the supine position after immobilization. To ensure reproducibility of daily positioning, the patients were instructed to keep their bladders full and bowels empty. CT images of the pelvis were obtained using axial CT (GE Healthcare, Chalfont St. Giles, U.K.), and clinical target volume (CTV) was contoured based on the location of surgical clips, preoperative imaging, operative findings, and/or surgical pathologies.
Planning target volume (PTV) was generated with a margin of 8-10 mm except posteriorly, where the margin was reduced to 5 mm. The superior margin was also tightened to exclude the small bowel from the high-dose radiotherapy zone. To measure movement of the prostate, the researchers placed surgical clips and measured their shifts in position relative to isocenter.
An IMRT plan was generated using a seven-field technique with Eclipse planning software (Varian Medical Systems, Palo Alto, CA). The prescribed doses ranged between 64 Gy and 68 Gy at 2.0 Gy per fraction depending upon whether the treatment was adjuvant or salvage therapy. The treatment plan treated at least 95% of the planning target volume to the prescribed dose.
All patients had orthogonal digitally reconstructed radiographs created from the treatment planning CT, the authors stated. Surgical clips were contoured and projected onto the radiographs for comparison with the surgical clips seen on the kV images obtained using the On-Board Imager system (Varian). Orthogonal (anterior-posterior and lateral) kV images were acquired daily to localize the prostate bed based on the clips, which were aligned relative to the reference isocenter on the planning radiographs.
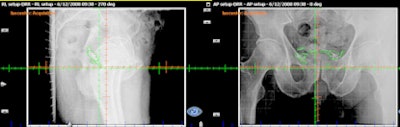 |
| With surgical clips used as a surrogate for the prostate bed, daily orthogonal images were acquired using an on-board imaging system to localize and align the prostate bed, based on clip location. Image courtesy of Dr. Ajay Sandhu from the University of California, San Diego. |
Shifts were measured from initial setup to bony anatomy, and the difference between the two readings was recorded as prostate bed motion, according to the authors. Shifts were recorded in the anterior-posterior, left-right, and superior-inferior directions on a daily basis.
Review of findings
Patient records of daily treatment and a three-month period following the conclusion of radiation therapy were reviewed for measurement of total error, setup error, and prostate bed motion, as well as for new symptoms presented by the patient during the surveillance period.
Total error, the sum of prostate bed motion and setup error, was defined as the change in position of the surgical clips on the orthogonal kV OBI compared to the original radiographic orthogonal images from the simulation CT.
Prostate bed motion -- the change in position of the prostate bed in relation to bony anatomy -- was evaluated using offline review software, which measured the displacement between surgical clips and bony anatomy. Measurement of inaccuracy in patient alignment using skin tattoos compared to alignment with bony anatomy reflected setup errors, the largest of which corresponded to obese patients.
The authors determined that prostate bed motion and setup error were measured in 384 orthogonal image pairs from 12 patients, and total error was measured in 692 orthogonal image pairs from the entire cohort.
Sandhu and colleagues believe that using IGRT in combination with surgical clips should enable clinicians to reduce treatment margins by 1-2 mm from those currently used when aligning to bony landmarks. Conversely, wider margins of 1-2 mm should be allowed when aligning treatment fields to bony landmarks.
"We recommend daily IGRT to enhance treatment precision for postprostatectomy patients requiring radiotherapy," they wrote.
By Cynthia Keen
AuntMinnie.com staff writer
June 25, 2008
Related Reading
Salvage radiotherapy for recurring prostate cancer enhances survival odds, June 17, 2008
Radiation therapy for prostate cancer linked to secondary cancers, May 28, 2008
CT planning eliminates need for urethrography in prostate, May 12, 2008
Trial results bolster hormone therapy plus radiation for prostate cancer, March 31, 2008
Disease-free survival, mortality uphold novel radiotherapies for prostate cancer, February 14, 2008
Copyright © 2008 AuntMinnie.com



















