In Part I of this article, Dr. Levon Nazarian, a professor and vice chairman of education at Thomas Jefferson University (TJU) Hospital in Philadelphia, focused on picking the right modality for imaging the upper extremities.
The second part of his talk highlighted exams of the hip, knee, ankle, and foot. As with the upper body, the choice of modality for musculoskeletal imaging should be undertaken with care.
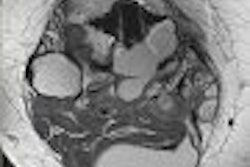
Hip
In a 2003 study, researchers looked at the clinical presentation and correlation between MR arthrography, ultrasound, and arthroscopy in 25 consecutive cases. They found that of the 17 patients whose flexion, abduction, external rotation (FABER) test results were reported at the time of examination, x-ray results were normal. Ultrasound turned in 100% specificity, but a dismal sensitivity of 13%. MRI also had 100% specificity but 31% sensitivity (Clinical Journal of Sports Medicine, May 2003, Vol. 13:3, pp. 152-156).
According to another paper, for hip effusion/iliopsoas bursitis, ultrasound diagnosed 100% of enlarged iliopsoas bursa, 56% of communication with hip joint, and 67% of hip effusion, while MRI diagnosed 100%, 100%, and 89%, respectively. The authors concluded that MR was the most accurate, although ultrasound was a cost-effective, fast, and easy alternative (European Radiology, February 2002, Vol. 12:2, pp. 409-415).
"I would caution you, though, that you really focus (ultrasound) to what it's good for, and for what it's not good for, go to radiographs and MRI immediately," Nazarian said.
In a 2005 study involving hip bursitis cases, researchers found that ultrasound diagnosed 100% of trochanteric bursitis, 45% of hip synovitis, 30% of iliopsoas bursitis, and 20% of ischiogluteal bursitis. MRI diagnosed 100%, 85%, 50%, and 20%, respectively (Clinical and Experimental Rheumatology, July-August 2005, Vol. 23:4, pp. 462-468).
"When you see hip synovitis, iliopsoas bursitis, other bursitis, you're going to want an MRI to be done first," he said.
In snapping hip syndrome, conventional radiography diagnosed 37%, while ultrasound alone found 46% in a 2001 study. Combining radiographs and ultrasound upped the figure to 83%. CT with another modality found 71%-94% of the cases, while MRI found 100% (European Radiology, September 2001, Vol. 11:9, pp. 1743-1747).
The authors recommended performing radiography and ultrasound, with MRI used for unresolved cases, Nazarian said.
Nazarian recommends MRI in most hip cases, with ultrasound utilized for tendon tears, tendinosis, and snapping hip syndrome.
Knee
In a 2005 study examining the quadriceps tendon, knee ultrasound was positive in all 28 patients. The authors recommended ultrasound for knee tendon injuries, Nazarian said (Knee Surgery, Sports Traumatology, Arthroscopy, October 2005, Vol. 13:7, pp. 564-568).
"This has been my experience too," he said. "Ultrasound just seems to be the way to go for that."
Ultrasound also performed well in a porcine knee cartilage in vitro study. For articular cartilage defects, ultrasound turned in 93%-94% sensitivity, 77%-90% specificity, 95%-98% positive predictive value, and 73%-78% negative predictive value (Radiology, June 2000, Vol. 215:3, pp. 846-851).
In a study looking at knees with osteoarthritis (OA), ultrasound diagnosed 100% of abnormal cartilages, 70% of effusion, 34% of synovial thickening, and 40% of popliteal cysts. MR diagnosed 99%, 85%, 50%, and 35%, respectively (Clinical Rheumatology, September 2003, Vol. 22:3, pp. 181-188).
In a comparison of MRI and ultrasound for medial meniscocapsular separation, ultrasound could demonstrate an MCL tear but not meniscocapsular separation (American Journal of Roentgenology, October 1998, Vol. 171:4, pp. 969-976).
The modality did perform well, however, in a 1996 study examining the medial collateral ligament, making the correct diagnosis in 15/16 (94%) patients with clinical MCL injury (Journal of Ultrasound in Medicine, September, 1996, Vol. 15:9, pp. 621-625).
"The problem is, when you're talking about ultrasound for the ligaments in the knee, it's often the associated injuries that are more important than the ligamentous tears you can see," he said. "You can be happy you made the MCL tear diagnosis, but then you can miss the more significant pathology. So that's why MRI should really be the gold standard for something like this."
For the knee, ultrasound is the test of choice for tendons, medial collateral ligament tear (for chronic cases), Baker’s cysts, and effusions. MRI should be the test of choice for pretty much everything else, including cruciate ligaments, menisci, fractures, and osteochondral injuries. The modalities are pretty comparable for femoral articular cartilage, Nazarian said.
Ankle/Foot
In a 1998 study evaluating ankle effusion, MRI detected as little as 1 mL of saline infused into cadaver ankles, while ultrasound detected 2 mL to 3mL and radiography detected 5 mL to 15 mL (AJR, May 1998, Vol. 170:5, pp. 1231-1238).
"This is a situation where MRI is the gold standard," he said. "Ultrasound is more sensitive, however, than radiography. So if you have somebody suspected of effusion, and if you see it with ultrasound, you're good. If you still need to identify fluid, then you can go to MRI."
For using ultrasound with painful Achilles tendon, anterior-posterior (AP) diameter correlated positively with pain, according to a 2003 study. Neovascularity correlated in 52%, with a specificity of 96%; spindle shape yielded 88% sensitivity and 64% specificity, while inhomogeneity showed 72% sensitivity and 84% specificity (Radiology, May 2003, Vol. 227:2, pp. 556-560).
In a 2001 study of Achilles tears, ultrasound was 100% sensitive, 83% specific, and 92% accurate for distinguishing partial from full thickness. Positive predictive value was 88%, while negative predictive value was 100% (Radiology, August 2001, Vol. 220:2, pp. 406-412).
"For a diagnostic test, you're not going to get much higher than these numbers," Nazarian said. ""This is why we say that ultrasound is the test of choice for the Achilles."
For peroneal subluxation, dynamic sonography had a positive predictive value of 100%, according to a 2001 study. Ultrasound and surgery had 100% agreement for tears of peroneus brevis and longus; subluxation was found in 20% of asymptomatic volunteers (AJR, October 2004, Vol. 183:4, pp. 985-988).
With the exception of the Achilles, the posterior tibial tendon (PTT) is the most commonly injured tendon in the ankle. In a 1998 study looking at ankle tendon pathology, ultrasound was 100% sensitive and 90% specific, compared with 23% sensitivity and 100% specificity for MRI (Foot & Ankle International, September 1998, Vol. 19:9, pp. 604-612).
In a 2002 study examining PTT tears, ultrasound was 83% sensitive and 90% specific. Ultrasound and MRI each turned in a 72% accuracy rate in a 2003 cadaver study of tears; ultrasound was 69% sensitive and 81% specific, while MRI was 73% sensitive and 69% specific (AJR, January 2002, Vol. 178:1, pp. 223-232) (Investigative Radiology, January 2003, Vol. 38:1, pp. 51-56).
"If there's a tie (in accuracy), then I'm going to want to do the ultrasound," Nazarian said.
For evaluation of PTT pathology, MRI and ultrasound were concordant in 100% of stage I PTT dysfunction, 73% of stage II, and 60% of stage III cases, according to a 2005 study. Overall concordance was 77% (Skeletal Radiology, July 2005, Vol. 34:7, pp. 375-380).
In a study examining the imaging of rheumatoid arthritis, ultrasound had a sensitivity of 79%, specificity of 97%, and accuracy of 96% for detecting metatarsophalangeal (MTP) erosions when compared with the gold standard of MRI. Radiography had a sensitivity of 32%, specificity of 98%, and accuracy of 93%. For MTP synovitis, ultrasound was 87% sensitive, 74% specific, and 79% accurate, compared with 43%, 89%, and 71%, respectively, for clinical exam (Arthritis & Rheumatism, July 2004, Vol. 50:7, pp. 2103-2112).
The accuracy of MRI and ultrasound for Morton's neuroma is similar and dependent on size, according to a 2003 study. Ultrasound had sensitivity of 85%-95% (Journal of Bone and Joint Surgery, September 2003, Vol. 85B:7, pp. 999-1005).
For the ankle/foot, Nazarian recommends ultrasound for tendons, ganglion cysts, Morton’s neuroma, dynamic studies, foreign bodies, and for screening of synovitis. MR is the preferred modality for fractures, osteochondral injuries, and osteomyelitis.
Nazarian said that his recommendations for musculoskeletal imaging will remain a work in progress.
"(The recommendations) are based on the data, my clinical experience, and what would I choose in a given instance," Nazarian said. "It's by no means set in stone, and this will evolve in time."
By Erik L. RidleyAuntMinnie.com staff writer
September 15, 2006
Related Reading
Part I: Choosing between MR and US in musculoskeletal imaging, September 7, 2006
From tears to TKA: The ins and outs of knee MRI, September 5, 2006
Color Doppler US shines for carpal tunnel syndrome, May 18, 2006
US with microconvex probes boost meniscal tear diagnosis, May 10, 2006
Focused exams suitable for some musculoskeletal US studies, March 26, 2006
Copyright © 2006 AuntMinnie.com